You’re staring into the toilet bowl. It’s a bit weird, right? But honestly, that quick glance before you flush is probably one of the most honest medical checkups you’ll ever have. Your gut doesn’t lie. It can’t. While we spend a fortune on wearable tech and blood panels, your body is literally handing you a daily status report for free.
The truth is that different types of poop and what it means for your longevity isn't just a conversation for doctors or parents of newborns. It’s for everyone. If you’ve ever noticed a sudden change in color or a texture that looks more like a topographical map than a smooth log, your body is trying to tell you something. Maybe it’s just the beets you had for dinner. Or maybe your gallbladder is waving a white flag.
Let's get into the nitty-gritty.
The Bristol Stool Scale: Why Shape Actually Matters
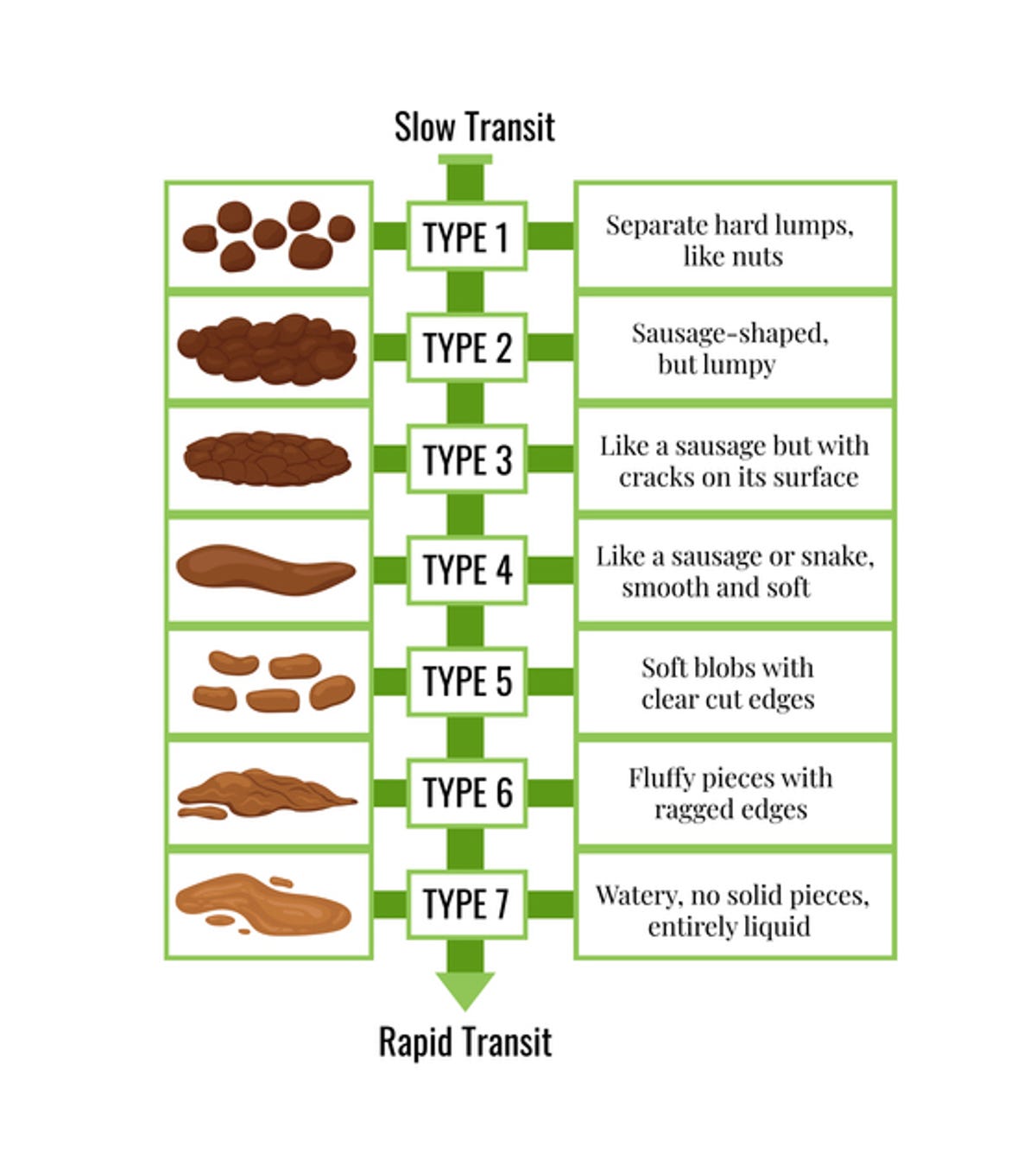
Back in 1997, a few researchers at the University of Bristol—most notably Dr. Stephen Lewis and Dr. Ken Heaton—realized we needed a universal language for bowel movements. They published a study in the Scandinavian Journal of Gastroenterology that basically changed how GI docs talk to patients. They created a seven-point scale. It’s not just academic fluff; it’s a roadmap for transit time.
Think of your colon like a high-speed rail system. If the train moves too slow, it gets dried out. If it moves too fast, it’s a watery mess.
If you’re seeing Type 1 or Type 2, you’re likely dealing with constipation. These are the hard, pebble-like lumps or the lumpy "sausage" shapes. They’re a sign that waste has spent way too much time in your large intestine, where water is constantly being sucked out. You’re likely dehydrated or lacking fiber. It hurts. It’s frustrating.
On the flip side, Type 6 and Type 7 are the "oh no, where’s the nearest bathroom" types. These are mushy, ragged, or entirely liquid. This means the waste flew through your system so fast that your body didn't have time to absorb the water or nutrients. This could be a viral bug, a food intolerance, or even just high stress.
The "Goldilocks" zone? That’s Type 3 and Type 4. Ideally, you want a smooth, soft sausage shape (Type 4). It should be easy to pass and leave you feeling empty. If you’re consistently in this zone, your transit time—the time from "mouth to south"—is likely sitting at a healthy 24 to 72 hours.
When Color Becomes a Warning Sign
Color is usually the first thing that makes people panic. Most of the time, it’s just diet. But sometimes, it’s a clinical red flag.
📖 Related: Why the EMS 20/20 Podcast is the Best Training You’re Not Getting in School
Most poop is brown because of stercobilin, a byproduct of broken-down red blood cells and bile. When bile (which is yellowish-green) travels through your gut, enzymes change it to that familiar brown.
Green is more common than you think
If it’s green, don't freak out immediately. Did you eat a massive kale salad? Did you drink a blue slushie? (Blue dye + yellow bile = green poop). However, if you haven't eaten anything green, it might mean "rapid transit." The bile didn't have enough time to turn brown because things are moving too quickly.
The scary colors: Red and Black
This is where we get serious. Bright red often means bleeding in the lower GI tract—think hemorrhoids or anal fissures. It’s common, but you should still get it checked. However, black, tarry stool (melena) is a different beast. This often indicates bleeding higher up, like an ulcer in the stomach or the esophagus. The blood gets "cooked" by stomach acid, turning it dark and sticky.
"If your stool looks like coffee grounds or black tar and has a metallic, foul smell, that’s an immediate phone call to your doctor," says Dr. Mark Pimentel, a leading gastroenterologist at Cedars-Sinai.
White or Pale: The Gallbladder Connection
If your poop looks like clay or white sand, you have a problem with bile. Either your liver isn't making enough, or your gallbladder/bile duct is blocked. Without bile, poop has no pigment. This is often accompanied by yellowing of the eyes (jaundice) or dark urine.
The Floater vs. Sinker Debate
You’ve probably heard that if it floats, it’s healthy. That’s actually a bit of a myth.
Most poop should sink. If it floats, it’s usually because of one of two things: excess gas or excess fat. If you’ve been eating a lot of beans or cruciferous veggies, the trapped air bubbles make the stool buoyant. No big deal.
But if it floats and looks greasy or oily, and it’s hard to flush away, that’s steatorrhea. This means your body isn't absorbing fats correctly. This can happen with Celiac disease, pancreatitis, or if your gallbladder is struggling. It’s a sign of malabsorption. You're eating the nutrients, but they're just sliding right through you.
👉 See also: High Protein in a Blood Test: What Most People Get Wrong
Why Your Poop Smells the Way it Does
Let's be real—it's never going to smell like roses. But there is a "normal" foul and an "abnormal" foul.
The standard scent comes from bacteria producing compounds like indole, skatole, and hydrogen sulfide. It’s the smell of a healthy microbiome doing its job.
However, if the smell is so pungent it stops you in your tracks, it might be an infection like Giardia or C. diff. People with ulcerative colitis or Crohn’s disease often report a very specific, metallic, or sickly-sweet odor during flares. If the smell changes drastically and stays that way for more than a week, it's worth noting.
The Hidden Influence of the Microbiome
We can't talk about different types of poop and what it means without mentioning the trillions of bacteria living in your colon. About 50% to 80% of the solid mass of your poop (excluding water) is actually bacteria—both living and dead.
When your microbiome is out of whack—a state called dysbiosis—your stool will reflect it. You might experience chronic bloating or "fragmented" stool that comes out in small pieces even if it’s soft. This is often seen in Irritable Bowel Syndrome (IBS).
Recent research from the American Gut Project suggests that people who eat more than 30 different types of plants per week have a much more diverse microbiome and, consequently, more "predictable" bowel movements. Variety isn't just the spice of life; it’s the fuel for your gut.
Frequency: How Often Should You Go?
There is a huge range for "normal." The medical rule of thumb is "three and three"—anywhere from three times a day to three times a week.
The key isn't the number; it’s the consistency. If you’ve gone once a day your entire life and suddenly you’re going four times a day, that’s a change. If you're straining every time, even if you go daily, you're technically constipated.
✨ Don't miss: How to take out IUD: What your doctor might not tell you about the process
Specific Scenarios: From Keto to Antibiotics
Your lifestyle choices show up in the bowl almost instantly.
- The Keto Poop: If you’re on a high-fat, low-carb diet, you might notice your stool is heavy, greasy, and maybe a bit yellowish. Without fiber to bulk it up, it can also become quite infrequent.
- The Antibiotic Effect: These drugs are like a nuclear bomb for your gut. They kill the bad guys, but they take out the good guys too. This often leads to "Type 7" liquid diarrhea. This is why doctors often recommend probiotics like Saccharomyces boulardii during a course of antibiotics.
- The Coffee Dash: Ever wonder why coffee makes you go? It’s not just the caffeine. Coffee stimulates the release of gastrin, a hormone that kicks the colon into high gear. It’s called the gastrocolic reflex.
Actionable Steps for Better Gut Health
If things aren't looking quite right, don't panic. Most issues can be course-corrected with small, intentional shifts.
Track the patterns. For three days, jot down what you ate and what the "result" looked like. You’ll start to see links. Maybe dairy is the reason you’re always a Type 6.
Hydrate by the numbers. Aim for half your body weight in ounces of water. If you’re Type 1 or 2, you are likely chronically dehydrated. Water is the lubricant of the digestive tract.
The Fiber Pivot. Don't just dump a bunch of fiber supplements into your diet overnight. That’s a recipe for gas pain and bloating. Increase slowly. Focus on "soluble" fiber (oats, avocados) to soften things up and "insoluble" fiber (wheat bran, veggie skins) to act as a broom.
Check your posture. Evolutionarily, we weren't meant to sit on a porcelain throne. We were meant to squat. Using a small footstool to lift your knees above your hips straightens the puborectalis muscle. This allows for a much easier exit.
Talk to a pro. If you see blood that isn't from a clear scratch, if you have unintended weight loss, or if your bowel habits change for more than two weeks, see a gastroenterologist. A colonoscopy is a minor inconvenience that saves lives.
Your digestive health is a mirror of your overall wellness. Listen to what it’s saying. Pay attention to the colors, the shapes, and the frequency. It’s the most direct feedback loop you have.
---