You’re sitting in the doctor's office, or maybe you just wrapped a cuff around your arm at the local pharmacy. The screen flashes. Your top number—the systolic—is a cool 118. Perfect. But the bottom number? It’s sitting at 94. You’ve been told for years that 120/80 is the "gold standard," so seeing that diastolic is high systolic is normal feels like a glitch in the system. It’s weirdly specific.
Most people obsess over the top number because that’s what we’re conditioned to do. We think of systolic pressure as the big hammer. But when that bottom number creeps up alone, doctors call it Isolated Diastolic Hypertension (IDH). It’s actually more common than you’d think, especially in younger adults or people who live under a mountain of stress.
High diastolic pressure isn't just a "minor" quirk. It’s your heart telling you that even when it’s resting between beats, the pressure in your pipes is still too high. Think of it like a garden hose. If you turn the nozzle off but the hose stays stiff and bulging, there’s a problem with the internal tension.
What’s Actually Happening Inside Your Arteries?
Blood pressure is a measurement of two distinct moments. The systolic (top) is the pressure when your heart pumps. The diastolic (bottom) is the pressure when your heart relaxes to refill with blood. If your diastolic is high systolic is normal, it means your arteries aren't relaxing the way they should. They are staying constricted, tight, and resistant even when the heart isn't actively pushing blood through them.
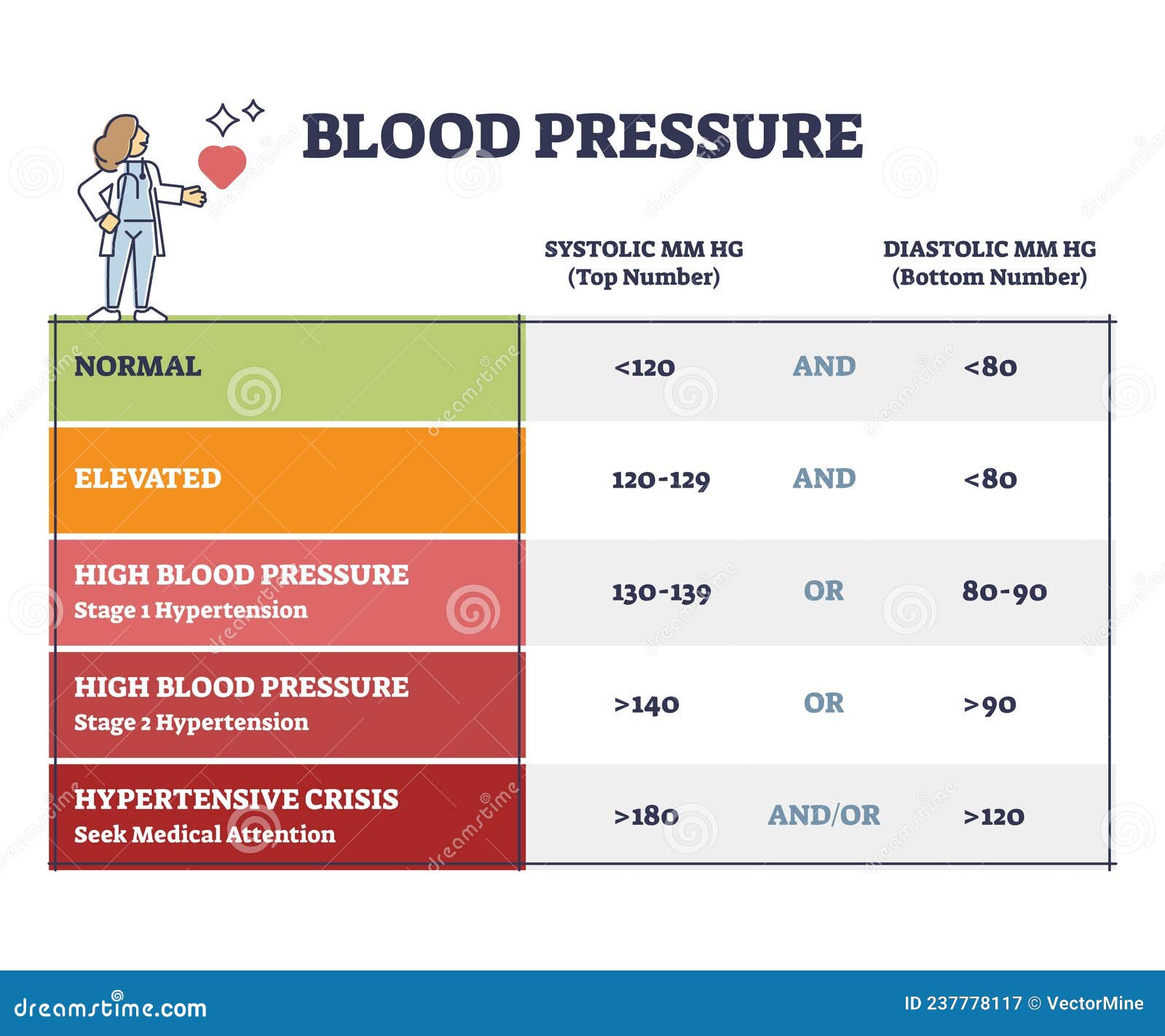
According to the American College of Cardiology, a diastolic reading of 80 mmHg or higher is technically Stage 1 hypertension, even if the top number is fine. When you hit 90 mmHg or above, you’re in Stage 2 territory.
Why does this happen? Usually, it's about total peripheral resistance. Your smaller blood vessels—the arterioles—are basically squeezing too hard. This forces the heart to work harder just to get blood into the chambers during that "rest" phase. It’s exhausting for your cardiovascular system. Honestly, it’s a bit like trying to fill a balloon that’s already half-inflated; you need more effort just to get started.
The Usual Suspects: Why the Bottom Number Spikes
It’s rarely just one thing. Often, IDH is the result of lifestyle choices that have caught up with your physiology.
✨ Don't miss: 2025 Radioactive Shrimp Recall: What Really Happened With Your Frozen Seafood
1. The Salt Factor
We know salt is bad, but for diastolic pressure, it’s a specific villain. Sodium makes your body hold onto fluid. More fluid means more volume in a closed system, which keeps that baseline pressure high.
2. Alcohol Consumption
This one is a sneaky trigger. While a glass of wine might relax you, alcohol actually increases the constriction of your blood vessels. Studies published in the journal Hypertension have shown a direct link between regular alcohol intake and elevated diastolic levels, even in people who have normal systolic readings.
3. Chronic Stress and "Always On" Mode
When you’re stressed, your sympathetic nervous system is firing like a machine gun. This keeps your blood vessels in a state of semi-contraction. If you’re a "type A" personality or work 60 hours a week, your body might literally forget how to dilate those vessels during the diastolic phase.
4. Sedentary Lifestyle
Your blood vessels are like muscles—they need to be "exercised" to stay flexible. If you sit at a desk all day, your vasculature can become stiff. Lack of movement leads to a decrease in nitric oxide production, which is the chemical your body uses to tell your arteries to relax.
Is It Actually Dangerous?
For a long time, researchers weren't sure if IDH was a big deal. They thought the systolic number was the only one that predicted heart attacks. We were wrong.
Recent data, including a massive study published in the New England Journal of Medicine, followed over 1.3 million people and found that while systolic pressure has a bigger impact, a high diastolic pressure independently increases the risk of "adverse cardiovascular events." Specifically, it’s a strong predictor of aneurysms and can contribute to long-term heart failure because the heart muscle thickens as it fights against that constant resistance.
🔗 Read more: Barras de proteina sin azucar: Lo que las etiquetas no te dicen y cómo elegirlas de verdad
There’s also the "conversion" factor. Many people with IDH eventually develop full-blown hypertension where both numbers are high. It’s basically a warning shot. Your body is giving you a chance to fix the plumbing before the whole system goes haywire.
The Role of Weight and Metabolic Health
Metabolic syndrome is often the "silent partner" when diastolic is high systolic is normal. If you have a bit of extra weight around the midsection, that visceral fat isn't just sitting there. It’s biologically active. It pumps out inflammatory cytokines that irritate the lining of your blood vessels (the endothelium).
When the endothelium is irritated, it can’t signal the vessel to relax. This is why you see high diastolic numbers in people who might otherwise look "healthy" but have poor metabolic markers, like high triglycerides or insulin resistance. It’s a systemic tension.
How to Lower That Bottom Number Naturally
The good news? Diastolic pressure is often more responsive to lifestyle changes than systolic pressure is. You can actually move the needle pretty quickly if you’re disciplined.
Focus on Potassium, Not Just Salt
Everyone tells you to cut salt. Few tell you to increase potassium. Potassium acts as a natural "buffer" to sodium. It helps your kidneys flush out excess salt and, more importantly, it helps ease the tension in your blood vessel walls. Eat more avocados, spinach, and beans. It’s basic, but it works.
The Power of Zone 2 Cardio
High-intensity interval training (HIIT) is great, but for diastolic health, "Zone 2" cardio is king. This is steady-state exercise where you can still hold a conversation—think brisk walking, light cycling, or swimming. Doing this for 30–40 minutes several times a week improves the elasticity of your arteries. It teaches them how to "open up" again.
💡 You might also like: Cleveland clinic abu dhabi photos: Why This Hospital Looks More Like a Museum
Magnesium Supplementation
Magnesium is basically nature’s calcium channel blocker. It helps the smooth muscles in your blood vessels relax. Many people are deficient because of modern soil depletion. A high-quality magnesium glycinate or malate can sometimes drop diastolic numbers by several points within a few weeks, though you should always check with a doctor first to make sure it doesn't clash with other meds.
Sleep Hygiene
Sleep apnea is a major, often undiagnosed, cause of high diastolic pressure. If you’re snoring or waking up tired, your oxygen levels might be dropping at night, causing a massive spike in adrenaline that keeps your pressure high well into the next day. Getting a sleep study could literally save your life.
When Should You Consider Medication?
If you’ve tried the diet, the walking, and the stress management, and your diastolic is high systolic is normal for months on end, it might be time for a pharmaceutical assist.
Doctors often lean toward ACE inhibitors or ARBs for this. These drugs specifically target the hormones that tell your blood vessels to constrict. By blocking those signals, the vessels can finally relax, and that bottom number drops.
Don't view medication as a failure. View it as a tool to prevent your heart from remodeling itself into a thicker, less efficient shape. Once the pressure is under control, many people find they can eventually taper off the meds if they maintain their lifestyle improvements.
Actionable Steps for Today
If you’ve just discovered your diastolic is high, don't panic. Panic just raises it further. Instead, do this:
- Validate the Reading: Home monitors are notoriously finicky. Take your pressure three times, five minutes apart, while sitting perfectly still with your back supported and feet flat on the floor. Average those three.
- Check Your Caffeine: Are you measuring after three cups of coffee? Caffeine is a vasoconstrictor. Try measuring first thing in the morning before your caffeine fix to see your "true" baseline.
- The 2-Week Sodium Purge: For 14 days, cut out processed foods, deli meats, and restaurant meals. Focus entirely on whole foods. If your diastolic drops significantly, you know you’re "salt-sensitive."
- Magnesium and Hydration: Start drinking at least 2 liters of water a day and consider a magnesium supplement. Dehydration makes your blood "thicker" and harder to pump, which can artificially inflate diastolic readings.
- Track the Trends: One high reading means nothing. A month of high readings means it’s time to see a cardiologist or a primary care physician to discuss a long-term plan.
Monitoring blood pressure isn't about hitting a perfect number every single time. It’s about the trend. If your diastolic is high systolic is normal, you’ve been given a clear signal that your vascular resistance is up. Address it now, and your 70-year-old self will thank you for not letting your arteries stay under tension for decades.