You’re sitting in the doctor’s office. The cuff tightens. It hums. Then the nurse rattles off two numbers, something like "120 over 80." Most of us focus on that first number because it's the loud one—the systolic pressure, the force of the heart's big squeeze. But honestly, that blood pressure lower number, known as diastolic pressure, is just as vital for understanding what’s happening inside your arteries. It’s the baseline. It’s the pressure in your system when your heart is actually catching its breath between beats.
If that lower number stays high, your heart never truly gets a break. Think about a garden hose that’s always under high tension, even when the nozzle is closed. Eventually, things start to leak or burst.
The Mystery of the Diastolic Baseline
The diastolic reading represents the minimum pressure in the arteries when the heart muscle rests between beats and fills with blood. For a long time, the medical community viewed this as the "lesser" of the two figures. You've probably heard more about the top number because it’s a massive predictor of stroke risk in older adults. But for people under 50, that blood pressure lower number is often a much more accurate crystal ball for future cardiovascular trouble.
When you see a reading like 85 or 90 for that bottom number, it means your peripheral resistance is up. Your tiny blood vessels are constricted. They're stiff. They aren't dilating like they should. Dr. George Bakris, a renowned hypertension specialist at the University of Chicago Medicine, has often pointed out that while systolic pressure tells us about the stiffness of the large arteries, the diastolic pressure is a window into the health of the smaller vessels.
It’s about the "load" your organs feel constantly.
Imagine your kidneys. They are delicate filters. If the "resting" pressure is always high, those filters are being pounded 24/7. There is no downtime.
When the Lower Number Acts Up Alone
Sometimes, you’ll see something weird: a normal top number but a high bottom number. Doctors call this Isolated Diastolic Hypertension (IDH). It’s actually quite common in younger, more muscular individuals or those carrying a bit of extra weight around the midsection.
✨ Don't miss: Egg Supplement Facts: Why Powdered Yolks Are Actually Taking Over
It’s frustrating. You feel fine. Your "big number" is 118. But the bottom is 92.
Why does this happen? Usually, it’s a sign of an overactive sympathetic nervous system. You're in "fight or flight" mode more than you realize. Maybe it’s the three shots of espresso you had at 10:00 AM, or perhaps it’s the chronic lack of sleep that has your body dumping cortisol and adrenaline into your system. This keeps those small vessels clamped down tight.
A study published in Hypertension (the journal of the American Heart Association) noted that while IDH used to be dismissed as a minor issue, we now know it significantly increases the risk of future heart failure. It’s a warning shot. Your body is telling you that the plumbing is starting to get stressed out before the main pump (the heart) shows major signs of wear and tear.
Salt, Alcohol, and the Silent Squeeze
We have to talk about sodium. It's the obvious villain, but the way it affects the blood pressure lower number is specific. Sodium makes you retain water. More water in the blood means more volume. More volume means higher pressure when the heart is at rest.
But alcohol is the "secret" culprit many people ignore.
A single night of heavy drinking can spike your diastolic pressure the next morning. If you're a "glass of wine every night" person, you might be keeping that lower number artificially inflated. Alcohol interferes with the baroreceptors—the sensors in your body that tell your brain how much pressure is in the pipes. When those sensors get "drunk" or desensitized, they let the pressure ride high.
🔗 Read more: Is Tap Water Okay to Drink? The Messy Truth About Your Kitchen Faucet
Potassium is the hero here. It’s basically the biological "anti-salt." It helps the walls of your blood vessels relax. If you aren't eating enough leafy greens, bananas, or potatoes, your vessels stay rigid. Rigid vessels mean a higher diastolic reading.
The Role of Weight and Sleep Apnea
If you’re carrying extra weight, your body has to build miles of new micro-vessels to supply that tissue. That's a lot of extra resistance.
Then there's the sleep factor.
Do you snore? Do you wake up tired? Sleep apnea is one of the most common "hidden" reasons for a stubborn blood pressure lower number. When you stop breathing at night, your oxygen levels drop. Your brain panics. It sends a massive jolt of adrenaline to wake you up so you don't, well, die. This happens dozens of times a night. That adrenaline keeps your diastolic pressure elevated long after you've woken up and started your day. If you can't get that bottom number down despite diet and exercise, a sleep study is often the missing piece of the puzzle.
Practical Steps to Ease the Pressure
Lowering that bottom number isn't just about taking a pill. It’s about changing the environment your blood vessels live in.
Watch the hidden salt. It’s not the salt shaker on your table. It’s the bread, the deli meats, and the canned soups. 70% of the sodium Americans consume comes from processed and restaurant foods. Check labels. If a serving has more than 400mg of sodium, put it back.
💡 You might also like: The Stanford Prison Experiment Unlocking the Truth: What Most People Get Wrong
Magnesium is your friend. Magnesium acts as a natural calcium channel blocker. It helps the smooth muscle cells in your arteries relax. Pumpkin seeds, almonds, and spinach are loaded with it. Some people find success with a high-quality magnesium glycinate supplement, but always check with your doctor first because magnesium can mess with certain medications.
Zone 2 Cardio. You don't need to sprint. In fact, heavy, straining weightlifting can sometimes spike diastolic pressure in the short term. Moderate, steady-state cardio—walking fast enough that you can still talk but would rather not—improves the elasticity of your blood vessels. Aim for 30 minutes, five days a week.
The "Breath Work" Hack. It sounds "woo-woo," but it’s pure physiology. Slow, deep breathing (around 6 breaths per minute) stimulates the vagus nerve. This flips the switch from the "stress" nervous system to the "relax" nervous system. Doing this for just 5 minutes twice a day can actually shave a few points off your diastolic reading over time.
Don't Panic, But Don't Ignore It
A single high reading doesn't mean you're in trouble. Stress, caffeine, and even the "white coat effect" of being in a clinic can send that blood pressure lower number soaring temporarily. The key is the trend.
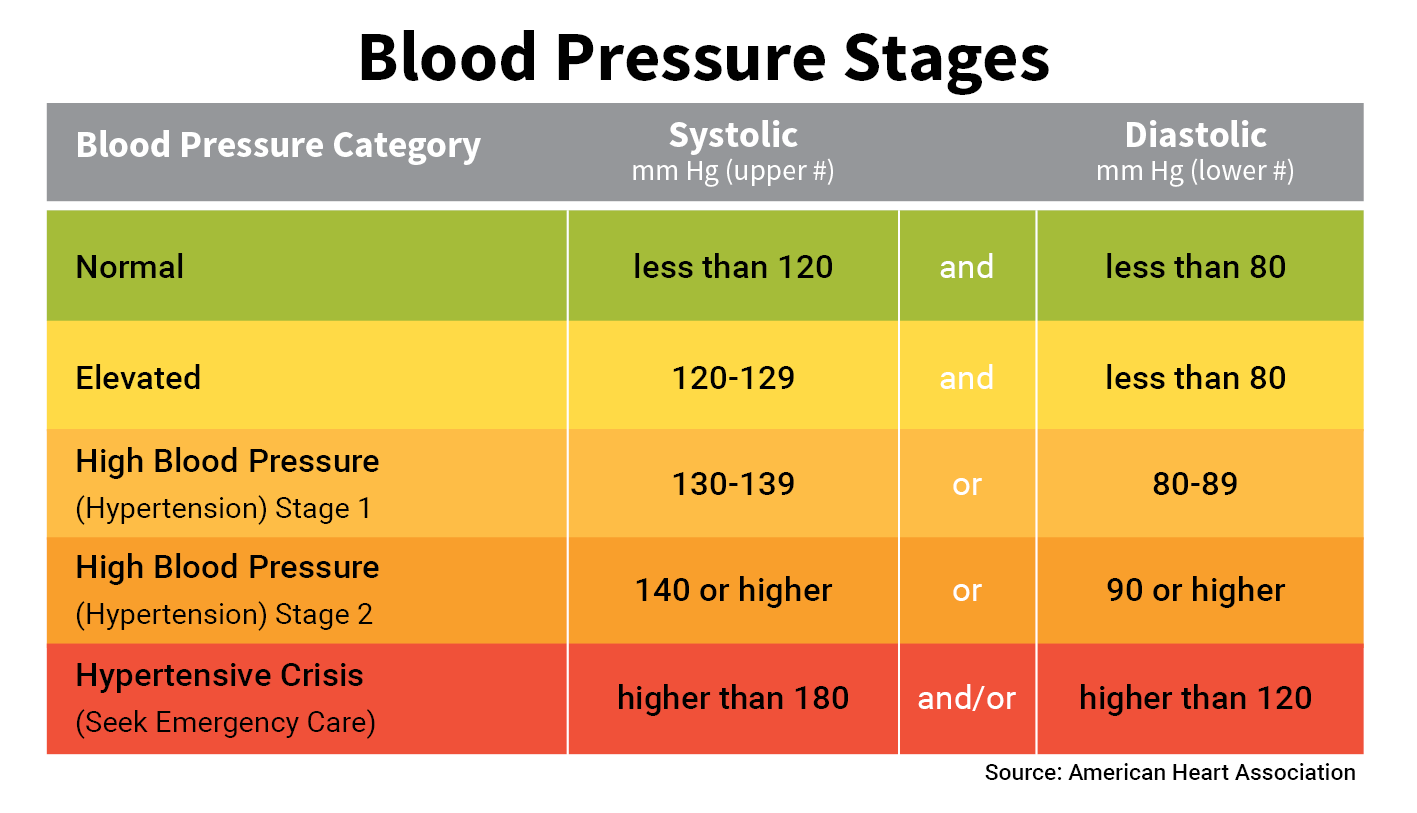
If you're consistently seeing a bottom number over 80, it's time to act. If it's over 90, it's an urgent conversation with your healthcare provider.
We used to think the diastolic number didn't matter as we aged. We were wrong. Maintaining a healthy baseline pressure ensures that your brain, kidneys, and heart are bathed in blood at a gentle flow rather than a high-pressure jet.
Your Action Plan
Start by tracking your numbers at home. Buy a validated upper-arm cuff (avoid the wrist ones; they're notoriously finicky). Measure your pressure in the morning before coffee and in the evening before bed. Keep a log for two weeks.
Bring this log to your doctor. It provides a much clearer picture than a single snapshot in a sterile office. Focus on increasing your potassium intake through whole foods and prioritizing seven to eight hours of quality sleep. Small, incremental shifts in your daily rhythm often do more for that lower number than any "crash" diet ever could. Consistent, quiet progress is what keeps the pressure down and the heart healthy for the long haul.