You’re sitting in the doctor’s office. The cuff squeezes your arm tight, then let's go with a rhythmic psst-psst-psst. The nurse rattles off two numbers, like 120 over 80. Most of us fixate on that first number—the systolic—because it feels like the big boss. It's the "high" number. But honestly, if you ignore dia in blood pressure measurements, you’re missing half the story of your heart’s health. That second number, the diastolic pressure, represents the pressure in your arteries when your heart is actually resting between beats.
Think about that for a second. Even when your heart isn't actively pumping, there is still pressure pushing against your vessel walls. If that pressure stays too high while the heart is trying to relax, things start to break down. It’s like a plumbing system that never gets a break from the water pressure; eventually, the pipes get brittle.
What "Dia" Actually Means for Your Arteries
The term "diastolic" comes from the Greek word diastole, meaning dilation or spreading out. It’s the phase of the cardiac cycle where the heart muscle relaxes and the chambers fill with blood. When we talk about dia in blood pressure, we are measuring the force exerted against the arterial walls during this specific refill period.
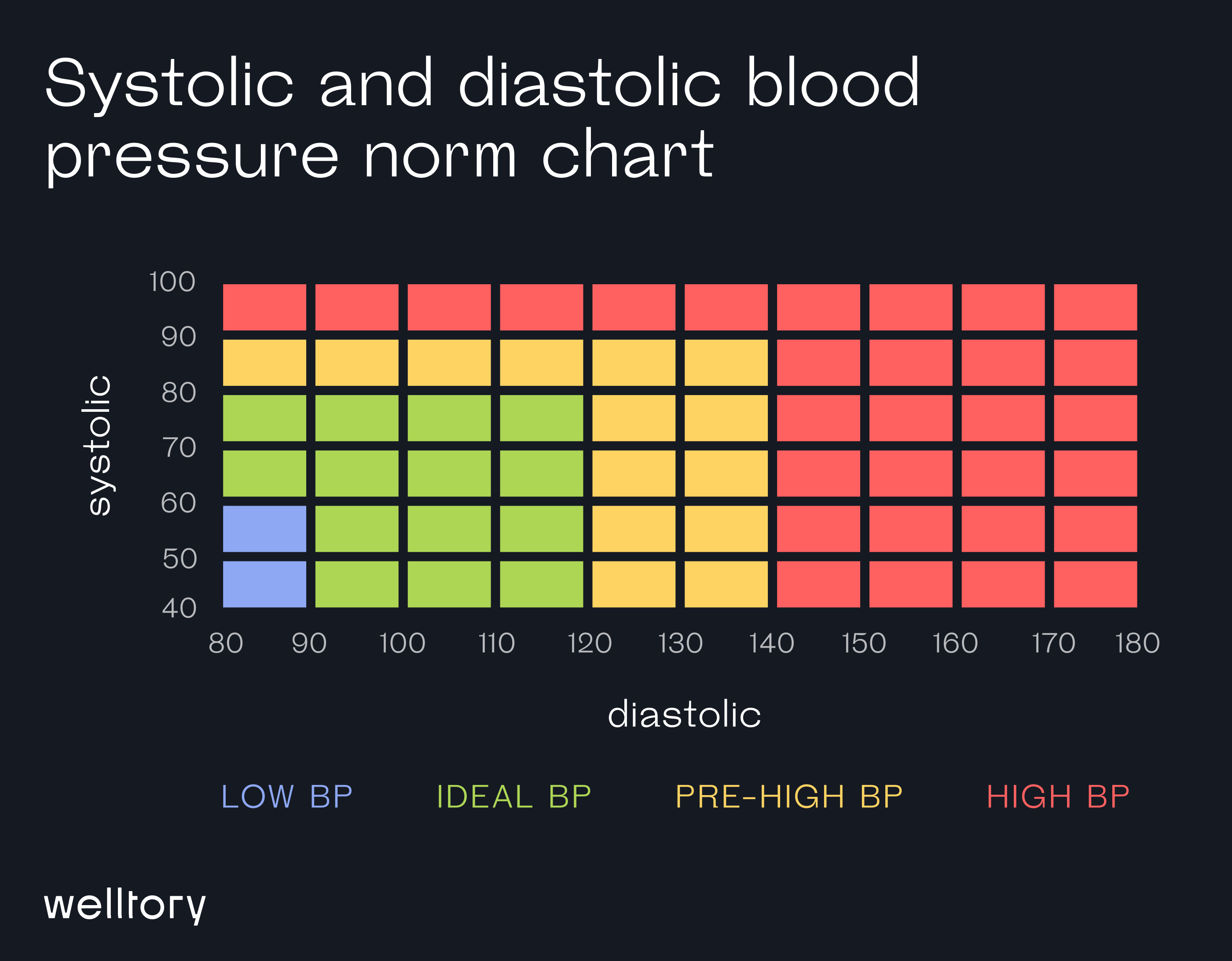
Medical experts at the American Heart Association (AHA) and the Mayo Clinic generally agree that a "normal" diastolic reading is under 80 mmHg. If you’re consistently hitting 80 to 89, you’ve entered Stage 1 hypertension territory. Hit 90 or higher? That’s Stage 2. It sounds like a lot of jargon, but basically, it means your arteries are under constant, unrelenting stress. They never get to "chill."
The physics of it is actually pretty wild. During systole (the top number), your heart is an active pump. During diastole, the "dia" part, the elastic recoil of your large arteries is what keeps the blood moving forward. If your arteries are stiff—a condition called atherosclerosis—they can’t recoil properly. This often leads to a spike in that bottom number, though interestingly, in much older adults, the diastolic can actually drop too low because the pipes are just too stiff to hold any pressure at all.
Why Young People Should Worry More About the Bottom Number
There’s this weird myth that only the top number matters. It’s outdated. While it’s true that systolic pressure is a massive predictor of cardiovascular risk in people over 50, younger adults—specifically those in their 20s, 30s, and 40s—often see "Isolated Diastolic Hypertension" (IDH).
📖 Related: How to Hit Rear Delts with Dumbbells: Why Your Back Is Stealing the Gains
IDH is when your top number is fine (say, 118), but your dia in blood pressure is high (like 92).
A major study published in JAMA (The Journal of the American Medical Association) tracked over 1.3 million people and found that while systolic pressure has a stronger overall link to heart attacks and strokes, diastolic pressure still significantly impacts the risk of adverse cardiovascular events. If you’re 35 and your diastolic is 95, you shouldn't just shrug it off because your systolic is 125. Your heart is working too hard during its "off" time. Over a decade or two, that constant "resting" pressure can thicken the heart muscle, leading to left ventricular hypertrophy. Basically, your heart gets too beefy in a bad way, making it less efficient at pumping.
The Sneaky Killers: Salt, Stress, and Sleep
Why does the diastolic number creep up? Honestly, it’s usually a mix of genetics and how we live.
- Sodium sensitivity: Some people are just salt-wasters, but others hold onto it. When you have too much salt, your body holds more water to dilute it. More fluid in the pipes equals more pressure, especially during the diastolic phase.
- The "Always On" Nervous System: If you’re constantly stressed, your sympathetic nervous system is firing. This keeps your blood vessels slightly constricted. Imagine trying to relax while someone is slightly squeezing a garden hose. That’s what stress does to your dia in blood pressure.
- Alcohol: This is a big one that people hate hearing. Regular alcohol consumption is one of the fastest ways to jack up diastolic pressure. It messes with the calcium levels in your arterial muscles, causing them to tighten up.
Sleep apnea is another massive contributor. If you’re snoring and stopping breathing at night, your oxygen levels drop. Your brain panics and sends a surge of adrenaline to wake you up. This causes a massive spike in blood pressure that often lingers well into the next day, specifically affecting the diastolic reading. If you feel tired all day and your bottom number is high, get a sleep study. Seriously.
Is "Too Low" a Problem?
We spend so much time talking about high blood pressure that we forget the "dia" can go too low. This is called diastolic hypotension. Generally, if that bottom number dips below 60 mmHg, it can be a problem, especially for the elderly.
👉 See also: How to get over a sore throat fast: What actually works when your neck feels like glass
Why? Because the heart’s own blood supply—the coronary arteries—actually fills up primarily during the diastolic phase. If the pressure is too low, the heart muscle itself might not be getting enough oxygenated blood. This can lead to dizziness, falls, and in extreme cases, it might even increase the risk of a heart attack because the heart is essentially "starving" for blood while it's trying to rest.
Real-World Nuance: White Coat Syndrome and Home Monitoring
Don't trust a single reading at the doctor's office. "White coat hypertension" is very real. You’re nervous, you’re in a sterile room, maybe you had to rush from the parking lot. Your dia in blood pressure might be 10 points higher than it is when you’re sitting on your couch watching Netflix.
The gold standard now is "Ambulatory Blood Pressure Monitoring" or at least consistent home testing.
When you test at home, follow the "Rule of Five":
- No caffeine or exercise for 30 minutes before.
- Sit with your back supported and feet flat on the floor (no crossing legs!).
- Keep your arm at heart level.
- Stay silent for 5 minutes before hitting the button.
- Take two or three readings a minute apart and average them.
This gives you a much truer picture of what your "dia" is doing when you aren't being poked and prodded by a medical professional.
✨ Don't miss: How Much Should a 5 7 Man Weigh? The Honest Truth About BMI and Body Composition
Taking Action: How to Bring the Number Down
If your diastolic is consistently high, you don't always have to jump straight to meds, though you should always follow your doctor's lead. Small shifts actually do make a massive difference.
The DASH diet (Dietary Approaches to Stop Hypertension) isn't just a gimmick; it’s one of the most studied interventions in medical history. It focuses on potassium, magnesium, and calcium. Potassium is like the "anti-salt." It helps your kidneys flush out sodium and actually relaxes the walls of your blood vessels. Potatoes (with the skin), bananas, spinach, and beans are your best friends here.
Magnesium is another "quiet" hero for dia in blood pressure. It acts like a natural calcium channel blocker, helping the smooth muscles in your arteries relax. Most people are actually deficient in it.
Then there’s zone 2 cardio. This isn't sprinting until you puke. It’s walking briskly or cycling at a pace where you can still hold a conversation but you’re definitely huffing a bit. This type of exercise improves "endothelial function"—the ability of your blood vessels to dilate and constrict when they’re supposed to.
Moving Forward With Your Health Data
Understanding the dia in blood pressure is about realizing that your heart deserves a break. High diastolic pressure is a sign of a body that can't "power down."
Your Next Steps
- Audit your salt intake for three days. Don't change anything, just track it. You’ll be shocked how much hidden sodium is in bread, sauces, and "healthy" frozen meals.
- Invest in a validated home cuff. Look for ones certified by the "Advancing Precision in Blood Pressure" (APBP) or similar organizations.
- Check your "resting" habits. If you’re drinking three glasses of wine every night, try cutting it to one or zero for two weeks and watch what happens to that bottom number. It usually drops faster than you’d think.
- Talk to your doctor specifically about the diastolic. Ask, "My systolic seems okay, but why is my diastolic hanging out in the 80s?" Force the conversation.
Monitoring your dia in blood pressure isn't just about avoiding a stroke in thirty years. It’s about how you feel today. When your pressure is in the optimal zone, you often have more energy, fewer headaches, and better overall circulation. Don't let the "bottom number" stay at the bottom of your priority list.