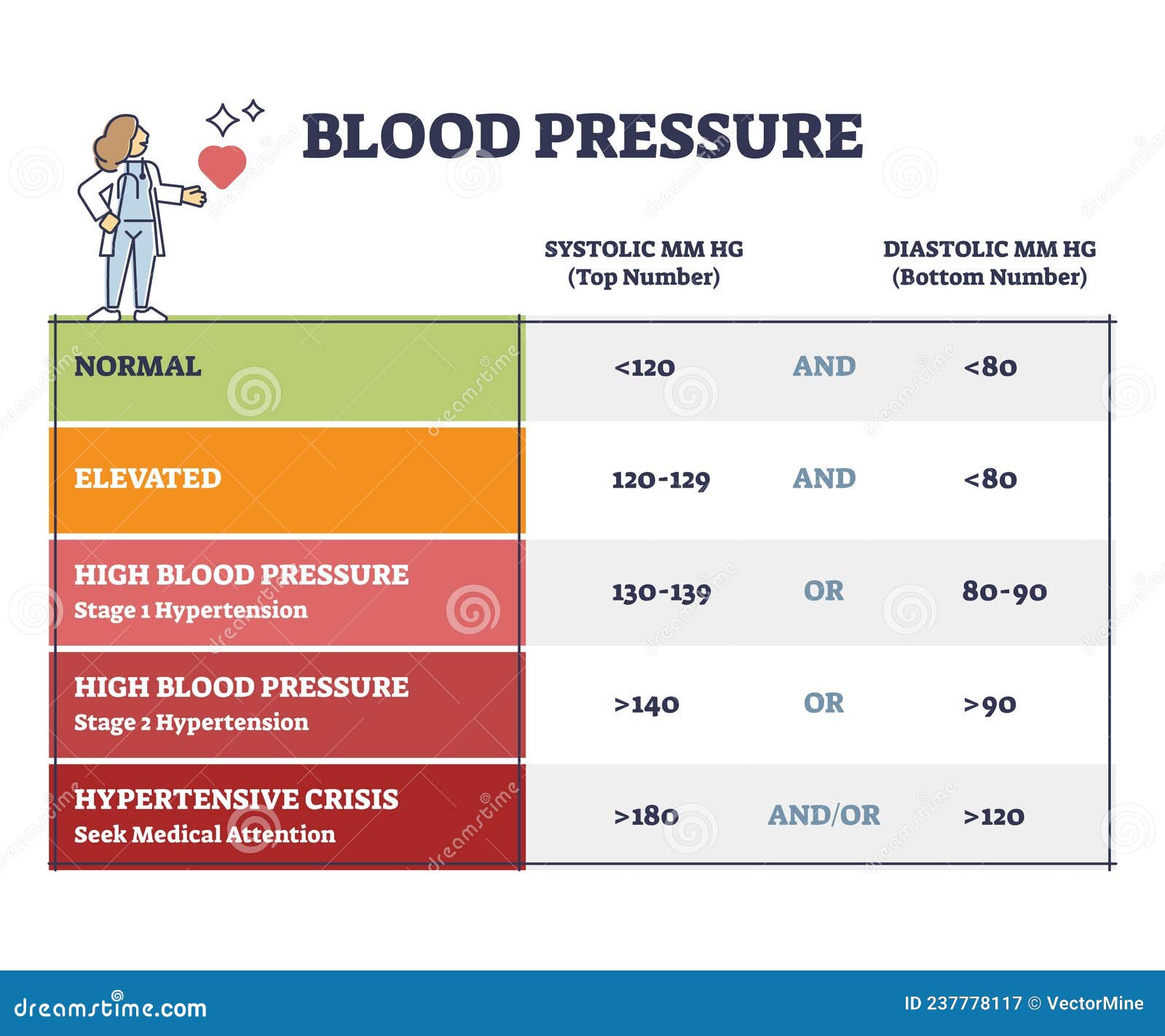
You just sat down at the pharmacy kiosk or left the doctor's office, and the screen flashed a number that felt a little heavy: 100. Specifically, that second number—the diastolic. Most people obsess over the top number (systolic), but when your diastolic blood pressure of 100 starts showing up consistently, the "wait and see" approach needs to end. It's high. Honestly, it's more than just "high"; in the medical world, it's the threshold for Stage 2 Hypertension.
Let's be real. It’s easy to ignore. You probably feel fine. High blood pressure is famously the "silent killer" because it doesn’t usually come with a cinematic headache or chest pain. But a bottom number of 100 means your heart is under constant pressure even when it's supposed to be resting between beats. Think of it like a garden hose that’s turned on full blast but has a kink in it. The pipes are straining.
What a diastolic blood pressure of 100 really means for your body
Blood pressure is a measurement of two distinct phases. The systolic (top) is the force when your heart pumps. The diastolic (bottom) is the pressure in your arteries when your heart rests between beats. When that bottom number hits 100 mmHg, your arteries are effectively never getting a break. They are under significant tension 24/7.
The American Heart Association (AHA) and the American College of Cardiology updated their guidelines a few years back, and they don't mince words about this. A diastolic reading of 90 or higher is Stage 2 Hypertension. If you're hitting 100, you've cleared that bar by a wide margin.
Is it an emergency? Usually, no—not if it's a one-off. But if you're sitting on the couch, relaxed, and it’s still 100? That’s a chronic stressor on your vascular system.
The physics of the "Resting" number
Imagine your circulatory system. Your heart beats about 100,000 times a day. If the "resting" pressure is 100, the arterial walls are being stretched and micro-damaged with every single second that passes. Over time, this leads to atherosclerosis. That’s just a fancy way of saying your pipes are getting stiff and scarred. When they get stiff, the pressure goes up even more. It’s a nasty feedback loop.
👉 See also: Brown Eye Iris Patterns: Why Yours Look Different Than Everyone Else’s
Why is your diastolic high while the top number might be okay?
Sometimes people see a "discordant" reading. Maybe your top number is 135 (not great, but not terrifying), but your diastolic blood pressure of 100 is staring you in the face. This is often called Isolated Diastolic Hypertension (IDH).
It’s actually more common in younger adults—people under 50. While older adults tend to see the top number skyrocket due to stiffening large arteries, younger people often have "tight" peripheral blood vessels.
- Stress and Caffeine: If you're running on triple espressos and deadline anxiety, your body releases cortisol and adrenaline. These hormones tighten the blood vessels.
- Alcohol: This is a big one. Regular drinking, even just a couple of beers a night, is a notorious driver of diastolic pressure.
- Salt Sensitivity: Some people's kidneys are just drama queens about sodium. They hold onto water, increasing the total volume of fluid in the pipes.
- Sedentary Lifestyle: If you spend 8 hours in a desk chair, your circulation isn't exactly thriving.
The real-world risks (No sugarcoating)
Let's look at the data. Dr. George Bakris, a renowned hypertension specialist at the University of Chicago Medicine, has often pointed out that while systolic pressure is a better predictor of stroke in older patients, a high diastolic is a massive red flag for younger people.
If you leave a diastolic blood pressure of 100 untreated for years, you’re looking at:
- Kidney Strain: The tiny blood vessels in your kidneys are delicate. High diastolic pressure shreds them. This can lead to chronic kidney disease before you even realize there's a problem.
- Vision Issues: Retinopathy happens when the vessels in your eyes leak or burst.
- Heart Failure: The heart has to push harder against that 100 mmHg "backpressure." Eventually, the muscle gets thick and stiff (Left Ventricular Hypertrophy). A thick heart is a weak heart.
Can you fix it without meds?
Maybe. It depends on how long it’s been high and what your "baselines" look like. If this is a new development, lifestyle changes can sometimes drop that number by 10 to 15 points.
✨ Don't miss: Pictures of Spider Bite Blisters: What You’re Actually Seeing
The Potassium Secret
Most people talk about cutting salt. That's fine. But adding potassium is often more effective. Potassium helps the kidneys flush out sodium and actually relaxes the walls of your blood vessels. Think bananas, sure, but also avocados, spinach, and sweet potatoes.
The "Zone 2" Cardio Effect
You don't need to run a marathon. In fact, sprinting might spike your pressure temporarily. What you want is "Zone 2" exercise—brisk walking or light cycling where you can still hold a conversation. Doing this for 30 minutes a day makes your blood vessels more "elastic." Elastic vessels mean lower diastolic pressure.
Sleep Apnea: The Hidden Culprit
If you snore or wake up feeling like a zombie, your diastolic blood pressure of 100 might be a nighttime problem. When you stop breathing during sleep, your oxygen drops, and your brain sends a panic signal to constrict your blood vessels. This "spikes" your pressure all night long, and it often stays high during the day.
When to see a doctor (and what they’ll do)
If you see 100 on the monitor once, don't panic. Sit quietly for five minutes. No phone. No talking. Feet flat on the floor. Take it again.
If it stays at 100 after three separate checks on different days, you need a professional opinion. A doctor will likely run a basic metabolic panel to check your kidneys and maybe an EKG.
🔗 Read more: How to Perform Anal Intercourse: The Real Logistics Most People Skip
Don't be scared of medication if they suggest it. Modern blood pressure meds like ACE inhibitors or ARBs are incredibly well-studied. They don't just "lower a number"; they protect your organs from the physical pounding of that 100 mmHg pressure. Sometimes, taking a low-dose pill for a year gives your system the "break" it needs while you work on losing weight or quitting smoking.
Actionable steps for right now
If you’ve confirmed a diastolic blood pressure of 100, start here:
- Buy a reliable home cuff: The Omron Platinum or something similar that is clinically validated. Kiosks at the grocery store are notoriously uncalibrated.
- Track for 7 days: Take your pressure in the morning and evening. Write it down. Doctors hate vague guesses; they love data logs.
- Cut the "hidden" sodium: It’s not the salt shaker; it’s the bread, the deli meat, and the canned soups.
- Increase Magnesium: Magnesium glycinate or citrate can help relax vascular smooth muscle.
- Check your meds: Are you taking Ibuprofen (Advil) or Decongestants (Sudafed) daily? These can jack up diastolic pressure significantly.
A diastolic of 100 is a message from your body. It's not a death sentence, but it is a "Check Engine" light that’s glowing bright red. Ignoring it is an option, but it’s an expensive one in the long run. Get the data, talk to a pro, and start moving. Your arteries will thank you in twenty years.
Immediate Next Steps:
- Stop all caffeine for 24 hours to see if your "resting" diastolic drops.
- Measure your BP tomorrow morning immediately after waking up and using the bathroom, but before eating.
- Schedule a baseline blood workup to check your creatinine and GFR levels; this ensures your kidneys haven't been impacted by the high pressure yet.