Most of us sit in that crinkly paper-covered chair at the doctor's office, wait for the cuff to squeeze our arm, and then tune out the moment the nurse says two numbers. We hear something like "120 over 80" and think, cool, I'm good. But if you ask the average person what that second number actually represents, you usually get a blank stare or some vague guess about "resting heart rate." It isn't that. Diastolic blood pressure meaning goes way deeper than just being the "bottom number." It’s actually a window into how well your blood vessels relax and how much pressure your heart is under when it's supposed to be taking a breather.
Think of it this way. Your heart is a pump that never gets a vacation.
When it beats, that’s the systolic pressure—the big push. But between those beats, your heart takes a micro-second break to refill with blood. That’s the diastolic phase. If the pressure in your arteries stays high even when the pump isn't pushing, you’ve got a problem. It’s like keeping a garden hose turned on full blast even when you aren't watering anything; eventually, the hose is going to leak or burst.
What's Really Happening During Diastole?
Basically, your heart is a muscle that needs to "refeed" itself. During the diastolic phase, the coronary arteries—the ones that supply the heart muscle itself with oxygen—actually do most of their work. If the diastolic blood pressure meaning in your specific case is "too high," it means your heart muscle isn't getting the relaxed environment it needs to soak up oxygenated blood.
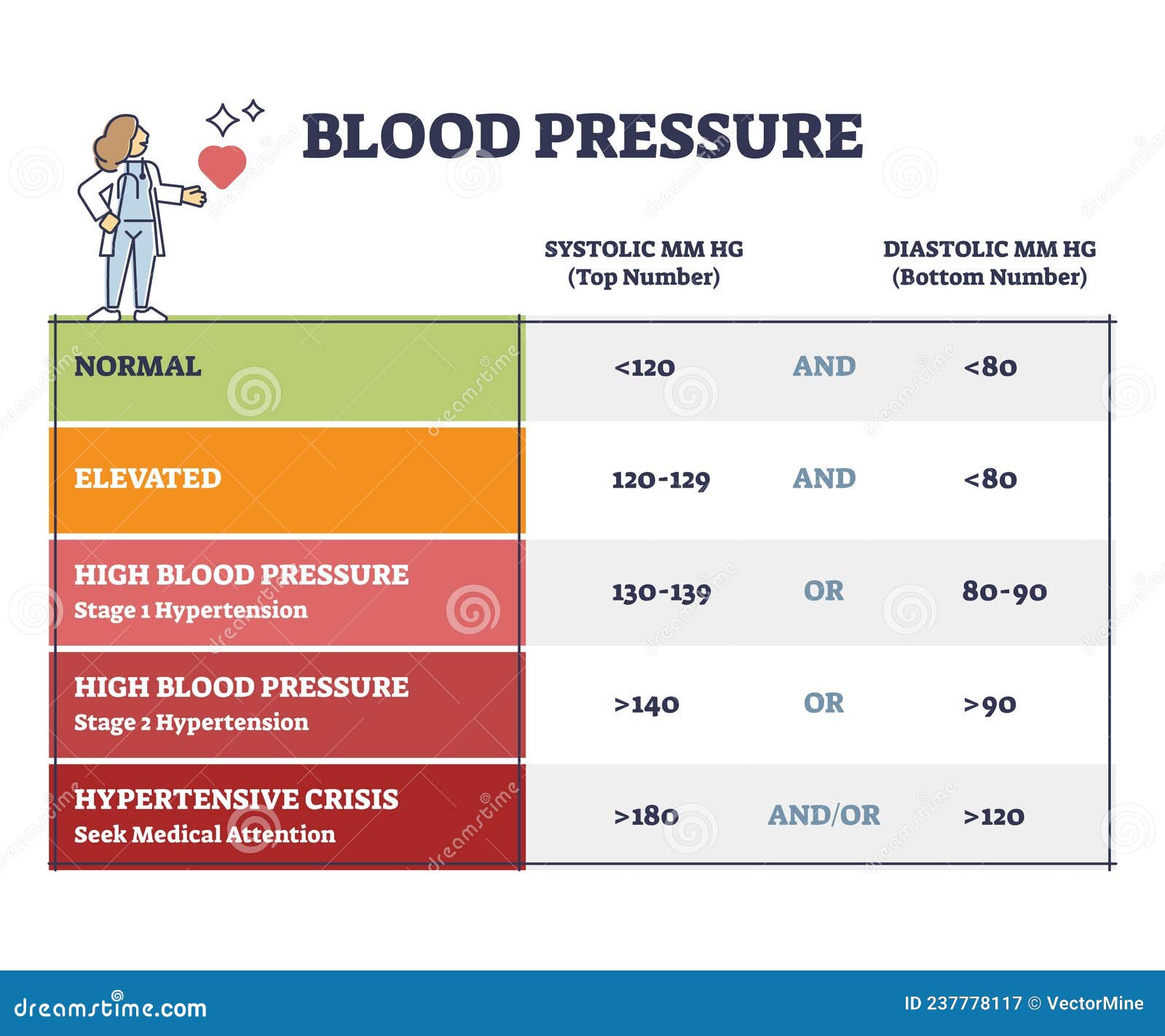
The American Heart Association defines a normal diastolic reading as less than 80 mmHg. If you’re consistently hitting 80-89, you’re in Stage 1 hypertension territory. Hit 90 or higher? That’s Stage 2. Honestly, many people walk around with a "perfect" top number but a creeping bottom number, and they have no idea they’re at risk for a stroke or heart failure. It’s a silent creep.
Doctors like Dr. Luke Laffin at the Cleveland Clinic often point out that while we used to obsess almost exclusively over the systolic (top) number—especially in older adults—the diastolic number is a massive predictor of cardiovascular issues in younger people. If you're 30 or 40 and your diastolic is high, your arteries are basically aging faster than you are. They're becoming stiff. They aren't "snapping back" the way healthy, elastic vessels should.
👉 See also: What Does DM Mean in a Cough Syrup: The Truth About Dextromethorphan
The Physics of Your Arteries
When the heart relaxes, your large arteries (like the aorta) use their elasticity to keep blood moving forward. It’s called the Windkessel effect. If your arteries are stiff from smoking, poor diet, or just bad genetics, they can't dampen the pressure. The pressure stays high. This puts a constant, grinding stress on the lining of your blood vessels, known as the endothelium. Once that lining gets damaged, it’s an open invitation for plaque to start building up.
Why Doctors Are Changing Their Minds About "Isolated" Diastolic Hypertension
You might hear someone say, "My top number is fine, it’s just the bottom one that’s high." This is what med schools call Isolated Diastolic Hypertension (IDH). For a long time, some clinics didn't treat IDH as aggressively as they did "regular" high blood pressure. But recent data, including a massive study published in the Journal of the American College of Cardiology, suggests that IDH is a serious warning sign.
It’s often a precursor.
You might have a normal systolic pressure today, but a high diastolic reading is often the "canary in the coal mine" for full-blown hypertension later. It’s also heavily linked to obesity and metabolic syndrome. If your body is carrying extra weight, especially around the midsection, your kidneys and nervous system often stay in a state of "high alert," which prevents the blood vessels from dilating properly during that diastolic rest phase.
What Messes With Your Diastolic Number?
It isn't just one thing. It's a messy cocktail of lifestyle and biology.
✨ Don't miss: Creatine Explained: What Most People Get Wrong About the World's Most Popular Supplement
- Salt intake: This is the obvious one, but people underestimate it. Sodium holds onto water. More water in your blood equals more volume. More volume in a fixed pipe equals more pressure. Simple physics.
- Alcohol: Kinda surprisingly, alcohol is a major trigger for diastolic spikes. It jacks up your sympathetic nervous system—your "fight or flight" mode.
- Sleep Apnea: If you snore or stop breathing at night, your oxygen levels drop. Your brain panics and sends a signal to tighten your blood vessels to keep blood moving to the brain. This keeps your diastolic pressure high even while you're sleeping.
- Stress: Chronic cortisol isn't just a buzzword; it physically narrows your peripheral blood vessels.
The Misconception of "Lower is Always Better"
While high pressure is the main villain, you can actually go too low. This is called diastolic hypotension. If your bottom number drops below 60 mmHg, you might start feeling dizzy or fatigued. Why? Because, as we mentioned earlier, the heart receives its own blood supply during diastole. If the pressure is too low, the blood doesn't have enough "oomph" to get into the small coronary arteries. This is a common issue for elderly patients who are over-medicated for hypertension. Their top number looks great, but their bottom number is so low they're fainting in the kitchen.
It’s a balancing act. You want the "Goldilocks" zone.
How to Get the Most Accurate Reading
Most people get "White Coat Hypertension." You walk into the clinic, see the doctor in the lab coat, and your blood pressure jumps 15 points. To truly understand your diastolic blood pressure meaning, you need home monitoring.
- Sit still. Don't talk. Don't look at your phone. Don't even think about that stressful email.
- Feet flat. Crossing your legs can artificially raise your pressure by several points.
- Cuff size matters. If you have muscular arms and use a standard cuff, the reading will be wrong. It’ll show as way higher than it actually is.
- Empty your bladder. A full bladder adds stress to the body, which—you guessed it—spikes the pressure.
Real-World Ways to Bring That Number Down
You don't always need a pill immediately, though you should always follow your doctor’s lead on that.
The DASH diet (Dietary Approaches to Stop Hypertension) is the gold standard here. It’s heavy on potassium. Potassium is basically the "anti-sodium." It helps your kidneys flush out salt and relaxes the walls of your blood vessels. Think bananas, sure, but also spinach, sweet potatoes, and white beans.
🔗 Read more: Blackhead Removal Tools: What You’re Probably Doing Wrong and How to Fix It
Exercise is the other big one. But not just "moving." Aerobic exercise—the kind that gets your heart rate up—teaches your blood vessels how to dilate. When you run or swim, your body releases nitric oxide. This is a gas that tells your arteries to "open up." Over time, regular exercise makes your arteries more "springy," which directly lowers that diastolic number.
The Psychological Component
We don't talk enough about the link between anxiety and diastolic pressure. If you're constantly in a state of "hyper-vigilance," your body never truly enters a state of rest. Your diastolic pressure is a reflection of your body's "baseline" tension. Practices like slow, diaphragmatic breathing aren't just for yogis; they physically stimulate the vagus nerve, which tells your heart and blood vessels to chill out.
Actionable Steps for Today
If you're staring at a high diastolic reading on your home monitor, don't panic. One reading is just a data point, not a diagnosis.
Start by tracking your numbers twice a day—once in the morning before coffee and once in the evening—for a full week. Bring that log to your doctor. Cut your sodium intake to under 2,300mg a day for two weeks and see what happens to the numbers. Often, that bottom number will respond surprisingly fast to dietary changes.
Finally, check your magnesium levels. Magnesium is a natural calcium channel blocker, meaning it helps the muscles in your blood vessels relax. Many people are deficient, and a simple supplement (after checking with a pro) can sometimes be the missing piece of the puzzle.
Immediate Next Steps:
- Purchase a validated arm-cuff blood pressure monitor (look for the "dabl Educational Trust" or "STRIDE BP" seal of approval).
- Begin a "Sodium Audit" for three days—actually read the labels on your bread, sauces, and canned goods.
- Schedule a 10-minute daily walk specifically after your largest meal to help with glucose and pressure regulation.
- Discuss the possibility of a Sleep Study with your physician if you experience daytime sleepiness or heavy snoring, as this is a hidden driver of high diastolic pressure.