You’re standing in the kitchen, or maybe you’re working in the garage, and suddenly—heat. Intense, searing heat. Your first instinct isn't to read a textbook. It's to grab your phone and look at degree of burns pictures to see if what you're looking at on your own skin matches the scary stuff on the screen. Honestly, it’s a terrifying way to spend five minutes.
The problem is that most of the photos you find online are either extreme medical cases or blurry, low-res snapshots that don't help you decide if you need an ER visit or just some cool water and a bandage. Looking at a screen while your arm is throbbing is stressful. Understanding the nuance between a nasty sunburn and a deep partial-thickness injury is what actually matters here.
Identifying the damage: Why degree of burns pictures often confuse people
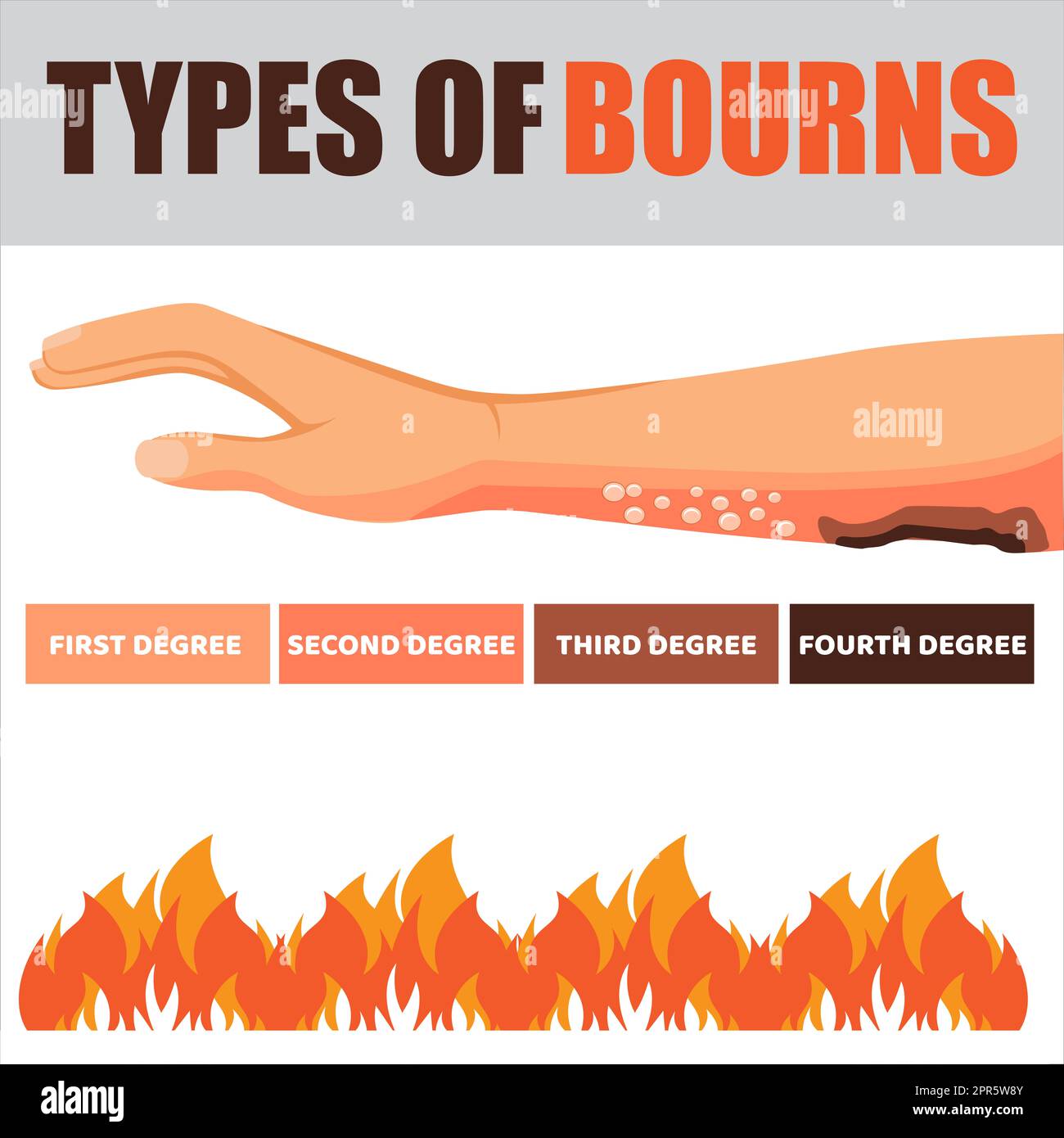
Most people think of burns in three neat categories. First, second, and third. Simple, right? Well, medical professionals like those at the Mayo Clinic or the American Burn Association actually prefer terms like "superficial" or "full-thickness." Why? Because a burn is a dynamic injury. It changes. What looks like a simple red patch at 2:00 PM might be a massive, fluid-filled blister by 6:00 PM.
If you're scrolling through degree of burns pictures, you’ll notice that first-degree burns look like a bad day at the beach. No blisters. Just red, dry skin. It hurts to touch, but it isn't "wet." But the moment you see a "wet" look or a blister, you’ve crossed the line into second-degree territory. This is where people get tripped up. They see a small blister and think, "Oh, it's just a small burn," ignoring the fact that the depth of the damage is what dictates the scarring and infection risk, not just the surface area.
The subtle trap of the "painless" burn
Here is the weirdest thing about looking at photos of severe burns. The ones that look the most horrific—white, charred, or leathery—are often the ones that don't hurt. If you find a picture of a third-degree burn, the skin might look like toasted parchment paper or even charred coal.
💡 You might also like: Resistance Bands Workout: Why Your Gym Memberships Are Feeling Extra Expensive Lately
If you have an injury that looks like that, and you can’t feel a thing when you touch it? That’s a medical emergency. The nerves are gone. They’ve been destroyed. Most folks see a lack of pain as a "good" sign, but in the world of burn triage, it’s a massive red flag.
Breaking down the visual cues
Let's get specific about what you are seeing when you look at these images.
First-Degree (Superficial):
Think of a classic sunburn. The skin is intact. It’s red. If you press your finger on it, the skin turns white (blanches) and then turns red again quickly. There is no "weeping" of fluid. These usually heal in about a week. You don't see many "scary" degree of burns pictures of these because they’re common and generally manageable at home.
Second-Degree (Partial-Thickness):
This is where the blisters live. These burns involve the epidermis and part of the dermis. The area looks moist. It’s a bright, angry red or may have mottled pink and white patches. It is incredibly painful. Air hitting a second-degree burn feels like a thousand needles. If you’re looking at pictures and seeing "shiny" skin, that’s the underlying dermis exposed.
📖 Related: Core Fitness Adjustable Dumbbell Weight Set: Why These Specific Weights Are Still Topping the Charts
Third-Degree (Full-Thickness):
These are the heavy hitters. The skin might be waxy white, leathery brown, or charred black. There are no blisters because the tissue is too damaged to even hold fluid that way. When you compare your injury to degree of burns pictures of third-degree burns, look for a lack of elasticity. The skin won't "bounce back" or change color when pressed.
When the location matters more than the look
You could have a second-degree burn the size of a postage stamp. Usually, no big deal. But if that stamp-sized burn is on your eyelid, your knuckle, or your genitals? That’s a different story entirely.
Experts at Johns Hopkins Medicine emphasize that burns on joints are tricky because as the skin heals, it tightens (contracture). If a burn heals poorly over your knuckle, you might lose the ability to fully close your hand. When looking at degree of burns pictures, people often focus on the "gross factor" rather than the location. If the burn is on a "functional" part of your body—hands, feet, face, or over a joint—you should probably have a professional look at it regardless of what the internet photos tell you.
Common myths that make things worse
There is so much bad advice out there. No, do not put butter on it. Please. Butter effectively "fries" the tissue by trapping the heat in.
👉 See also: Why Doing Leg Lifts on a Pull Up Bar is Harder Than You Think
- Ice is also a bad idea. It sounds counterintuitive, but ice can actually cause frostbite on top of a burn or constrict blood flow so much that the tissue dies.
- Don't pop the blisters. I know it’s tempting. But that blister is a sterile "natural bandage" created by your body. The moment you pop it, you’ve opened a highway for bacteria.
- Skip the toothpaste. It’s not a cooling agent; it’s a chemical irritant.
When you look at degree of burns pictures of infected wounds, they often started as a simple second-degree burn that someone tried to treat with a "home remedy" they found on a forum. Infection looks like spreading redness (cellulitis), pus, or a foul smell. If the redness is moving away from the burn site like a growing map, get to a doctor.
The 10% Rule and the "Rule of Nines"
Medical pros use something called the Rule of Nines to figure out how much of the body is affected. It’s a bit technical, but basically, your palm (including fingers) represents about 1% of your total body surface area.
If you're comparing your injury to degree of burns pictures and you realize the affected area is larger than 10% of your body (about 10 of your palms), you are at risk for systemic shock. Your body loses fluid through those burn sites. It’s not just about the skin; it’s about your kidneys and your blood pressure.
What to do right now: Actionable Steps
Stop looking at the pictures for a second and do these things if the burn just happened:
- Run cool (not cold) water over the area for at least 10 to 20 minutes. This stops the "cooking" process. Even after you move away from the heat source, the layers of skin are still holding that thermal energy.
- Remove jewelry immediately. If your finger starts to swell and you have a ring on, that ring becomes a tourniquet. You do not want to lose a finger because of a wedding band.
- Cover loosely. Use a sterile gauze bandage or, in a pinch, clean plastic wrap. Plastic wrap is actually great because it doesn't stick to the wound and keeps air off those sensitive nerve endings.
- Assess the "Big Three." Is it larger than three inches? Is it on the face, hands, or feet? Does it look charred or white? If the answer to any of those is "yes," go to urgent care or the ER.
If the burn is chemical, you need to flush it for much longer—sometimes 30 minutes or more—and check the MSDS (Material Safety Data Sheet) if it happened at work. Electrical burns are even more deceptive. You might see a tiny "entry" and "exit" wound on the skin that looks like a minor first-degree burn, but the electricity may have caused internal damage to your heart or muscles on its way through.
The takeaway? Use degree of burns pictures as a rough guide, but trust your gut. If it’s weeping, if it’s numb, or if it’s bigger than your hand, stop Googling and start driving to a clinic. Proper wound care in the first 24 hours is the difference between a faint memory and a permanent scar.