It starts with that tiny, nagging tingle. You’re sitting at your desk or out for dinner, and suddenly, you realize you have to go. Again. Then comes the burning—that sharp, stinging sensation that makes you dread the bathroom. If you’ve been there, you aren’t alone. Roughly 60% of women will deal with at least one urinary tract infection in their lifetime. It’s annoying. It’s painful. Honestly, it’s a massive disruption to your life.
But why does it happen so often? Understanding the common causes of uti in females isn't just about bad luck. It's about biology, lifestyle choices, and sometimes, things as simple as the clothes you wear or the way your body is built.
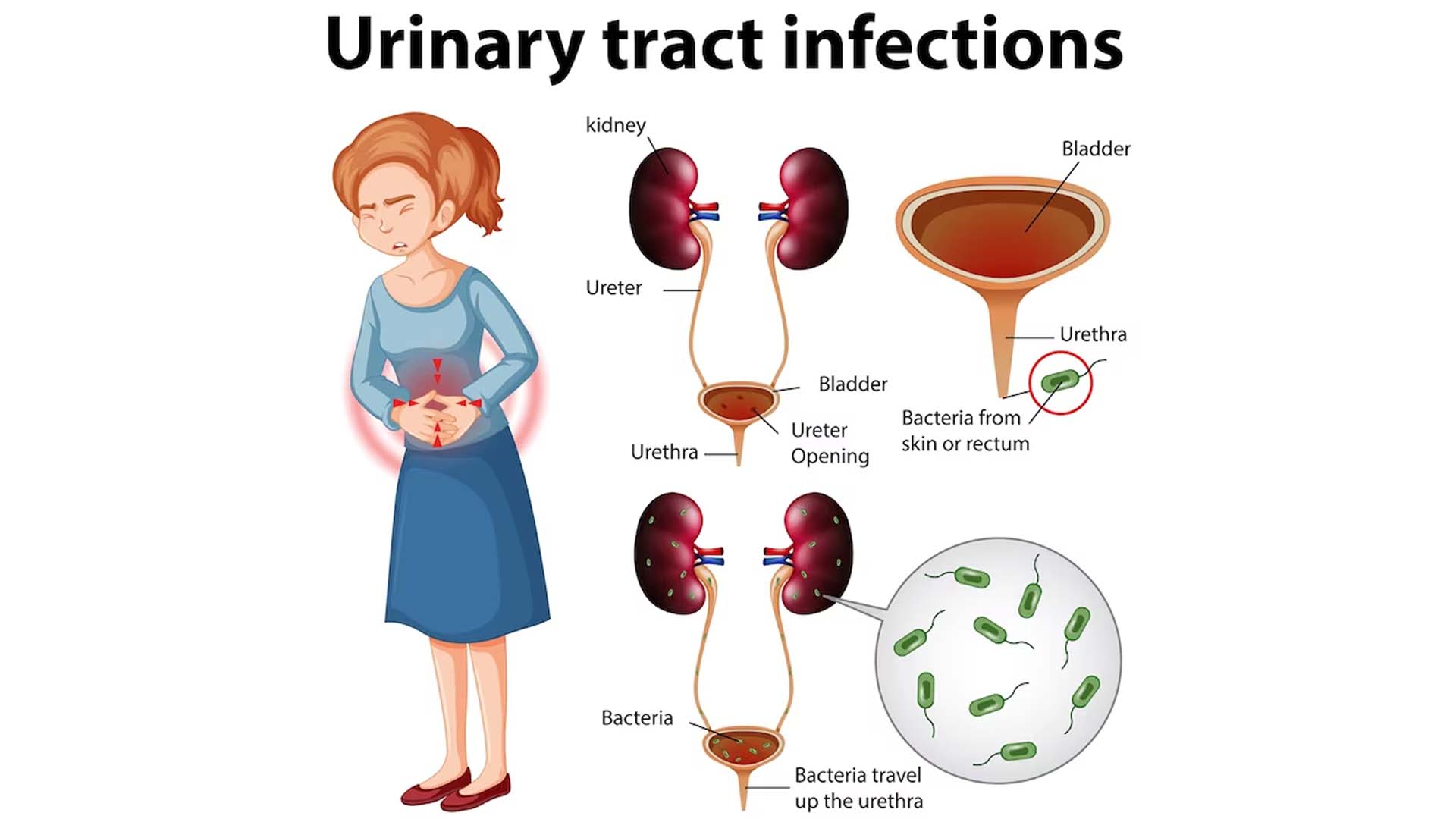
Most people think it’s just about "being dirty." That’s a myth. You can be the most hygienic person on the planet and still end up with a prescription for nitrofurantoin. It’s more about the migration of bacteria—specifically Escherichia coli (E. coli)—from places it belongs to places it definitely does not belong.
The Anatomy Factor: Why Being Female Makes a Difference
Biology really didn't do us any favors here. The female urethra is short. We’re talking maybe 1.5 inches long. Compare that to the male urethra, which can be up to 8 inches. Because the distance is so short, bacteria like E. coli have a much easier "commute" to the bladder. Once they get in there, they latch onto the bladder wall and start multiplying.
Distance matters. In females, the urethra is located very close to the anus. This is the primary reason why "wiping front to back" is the first thing every doctor tells you. It’s basic geography. If you move bacteria from the rectal area toward the urethral opening, you’re essentially inviting an infection.
Sexual Activity and the Honeymoon Cystitis Phenomenon
It’s an uncomfortable topic for some, but sex is one of the most frequent triggers. There’s even an old-school term for it: "honeymoon cystitis." During intercourse, physical movement can push bacteria into the urethra. It doesn't mean anyone is "unclean." It’s just mechanical.
If you find yourself getting a UTI every time you're intimate, it might be due to a few things. Friction can cause micro-irritation in the urethral opening, making it easier for bacteria to stick. Using spermicides or certain types of diaphragms can also change your vaginal flora. When the "good" bacteria (Lactobacillus) get killed off, the "bad" bacteria take over.
🔗 Read more: How to Eat Chia Seeds Water: What Most People Get Wrong
Urinating after sex is the golden rule. It’s basically a natural flush system. If you wait hours or go to sleep immediately, those bacteria have all night to climb up into your bladder and set up shop.
The Role of Hormones and Menopause
Hormones aren't just for mood swings; they play a massive role in your urinary health. Estrogen is a protector. It keeps the tissues of the vagina and urethra thick, elastic, and acidic. This acidity is what keeps the bad bacteria at bay.
When women hit menopause, estrogen levels crater. The tissues thin out—a condition called vaginal atrophy. The pH balance shifts. Suddenly, the protective barrier is gone, and the urinary tract becomes much more susceptible to colonization. This is why many postmenopausal women find themselves dealing with chronic, recurring UTIs for the first time in their lives. Dr. Elizabeth Kavaler, a urological surgeon, often points out that localized estrogen cream can sometimes be more effective at preventing these infections than repeated rounds of antibiotics.
Birth Control Choices You Might Not Suspect
Not all birth control is created equal when it comes to your bladder. Spermicides are a major offender. They contain a chemical called nonoxynol-9. While it’s great at killing sperm, it’s also a "scorched earth" chemical for your vaginal microbiome. It kills the Lactobacillus that keeps your pH balanced. Without that acidic environment, E. coli thrives.
Diaphragms can also be a culprit. They can sometimes press against the urethra, making it harder to empty your bladder completely. If urine sits in the bladder for too long—what doctors call "stasis"—it becomes a literal petri dish for bacteria.
Common Causes of UTI in Females: Dehydration and Holding It
We’ve all been there. You’re in a long meeting or on a road trip, and you decide to "just hold it." Big mistake. Your bladder is designed to be flushed regularly. When you hold urine, you’re giving any bacteria that managed to sneak in a chance to multiply.
💡 You might also like: Why the 45 degree angle bench is the missing link for your upper chest
Bacteria double roughly every 20 minutes. If you wait four hours to pee when you really needed to go, you’ve allowed several generations of bacteria to bloom.
Dehydration makes it worse. When you aren't drinking enough water, your urine becomes concentrated and dark. This concentrated urine is irritating to the bladder lining. More importantly, you aren't peeing often enough to clear the system. Think of your urinary tract like a plumbing system; if the water isn't flowing, the pipes get gunky.
Hygiene Products and the "Cleanliness" Trap
There is a multi-billion dollar industry dedicated to making women think their bodies should smell like a "spring meadow." Scented soaps, douches, "feminine wipes," and bubble baths are often cited as common causes of uti in females.
The vagina is self-cleaning. When you introduce harsh chemicals or fragrances, you disrupt the delicate bacterial balance. This irritation can inflame the urethra, making it significantly easier for an infection to take hold. Stick to plain water or very mild, unscented soap for the external areas only. If a product says "scented," stay away from it.
Underlying Health Conditions and Genetics
Sometimes, you do everything right and still get sick. It feels unfair. Some women are simply genetically predisposed to UTIs. Research has shown that some people have certain types of receptors on their bladder cells that bacteria can "velcro" onto more easily than others. If your mother had chronic UTIs, you might be more likely to have them too.
Diabetes is another major factor. High blood sugar means there is more glucose in your urine. Bacteria love sugar. It’s essentially high-energy fuel for an infection. Furthermore, diabetes can sometimes cause nerve damage that prevents the bladder from emptying fully, leading to the "stasis" problem mentioned earlier.
📖 Related: The Truth Behind RFK Autism Destroys Families Claims and the Science of Neurodiversity
Kidney stones or an enlarged "kink" in the ureter can also block the flow of urine. Anything that prevents the total and frequent evacuation of the bladder is a risk factor.
Can Your Clothes Actually Cause a UTI?
It sounds like an old wives' tale, but there’s some truth to it. Tight-fitting clothing, especially synthetic fabrics like polyester or nylon, traps moisture. Bacteria love warm, damp environments.
Cotton underwear is the standard recommendation for a reason. It breathes. If you’re wearing thongs, there’s an even more direct path for bacteria to migrate from the back to the front. It’s not that you can never wear leggings or lace, but if you’re prone to infections, switching to breathable fabrics can make a noticeable difference in your "microclimate."
Antibiotic Resistance: The Growing Challenge
One of the biggest issues experts like those at the Mayo Clinic are seeing now is antibiotic resistance. For decades, we treated every UTI with the same few drugs. Now, some strains of E. coli have learned how to fight back.
If you take an antibiotic and your symptoms don't clear up, or if they come back a week later, you might be dealing with a resistant strain. This is why "self-treating" with leftover pills from a friend is a terrible idea. You need a culture to see exactly what bacteria you have and which drug will actually kill it.
Actionable Steps to Stop the Cycle
If you are tired of the constant "fire" in your bladder, you need a proactive strategy. It isn’t just about one thing; it’s about a lifestyle shift.
- Hydrate like it's your job. Aim for enough water that your urine is consistently pale yellow. This keeps the "flushing" mechanism active.
- The "Post-Coital" Flush. Make it a non-negotiable habit to urinate within 15 minutes of sexual activity.
- Re-evaluate your birth control. If you use spermicides and get frequent UTIs, talk to your doctor about switching to an unlubricated condom or a different method entirely.
- Wipe correctly. It sounds basic, but many people get lazy. Front to back. Every. Single. Time.
- Check your supplements. There is some evidence that D-Mannose (a type of sugar found in cranberries) can help prevent E. coli from sticking to the bladder walls. It’s not a cure once you have an infection, but it can be a solid preventive measure.
- Avoid the "scents." Throw away the scented tampons, the douches, and the floral-scented body washes. Your bladder will thank you.
- Get a culture. If you get more than three UTIs a year, don't just take the "standard" pill. Ask your doctor for a formal urine culture to identify the specific bacteria and check for resistance.
Managing the common causes of uti in females requires a mix of biological awareness and daily habits. While you can't change your anatomy, you can change the environment that allows bacteria to thrive. If symptoms persist or you develop back pain and fever, see a doctor immediately, as this can indicate the infection has moved to your kidneys, which is a much more serious medical situation.