When you first get the news—that positive ANA test, the butterfly rash, the crushing fatigue—the very first thing your brain does is jump to the darkest possible corner. You wonder if this is a death sentence. You've probably googled it at 3:00 AM. Can you die from lupus? Honestly, the short answer is yes, but it’s nowhere near as common as it was fifty years ago, and the context matters more than the "yes" itself.
Back in the 1950s, the five-year survival rate for Systemic Lupus Erythematosus (SLE) was under 50%. People were terrified for a reason. Today? More than 90% of people diagnosed with lupus live for at least ten years, and many live a full, normal lifespan. But we have to be real about the risks because "manageable" doesn't mean "harmless." Lupus is a shapeshifter. It doesn't just make you tired; it can quietly attack your kidneys, your heart, or your brain while you think you're just having a "bad day."
Understanding the Stakes: How Lupus Becomes Life-Threatening
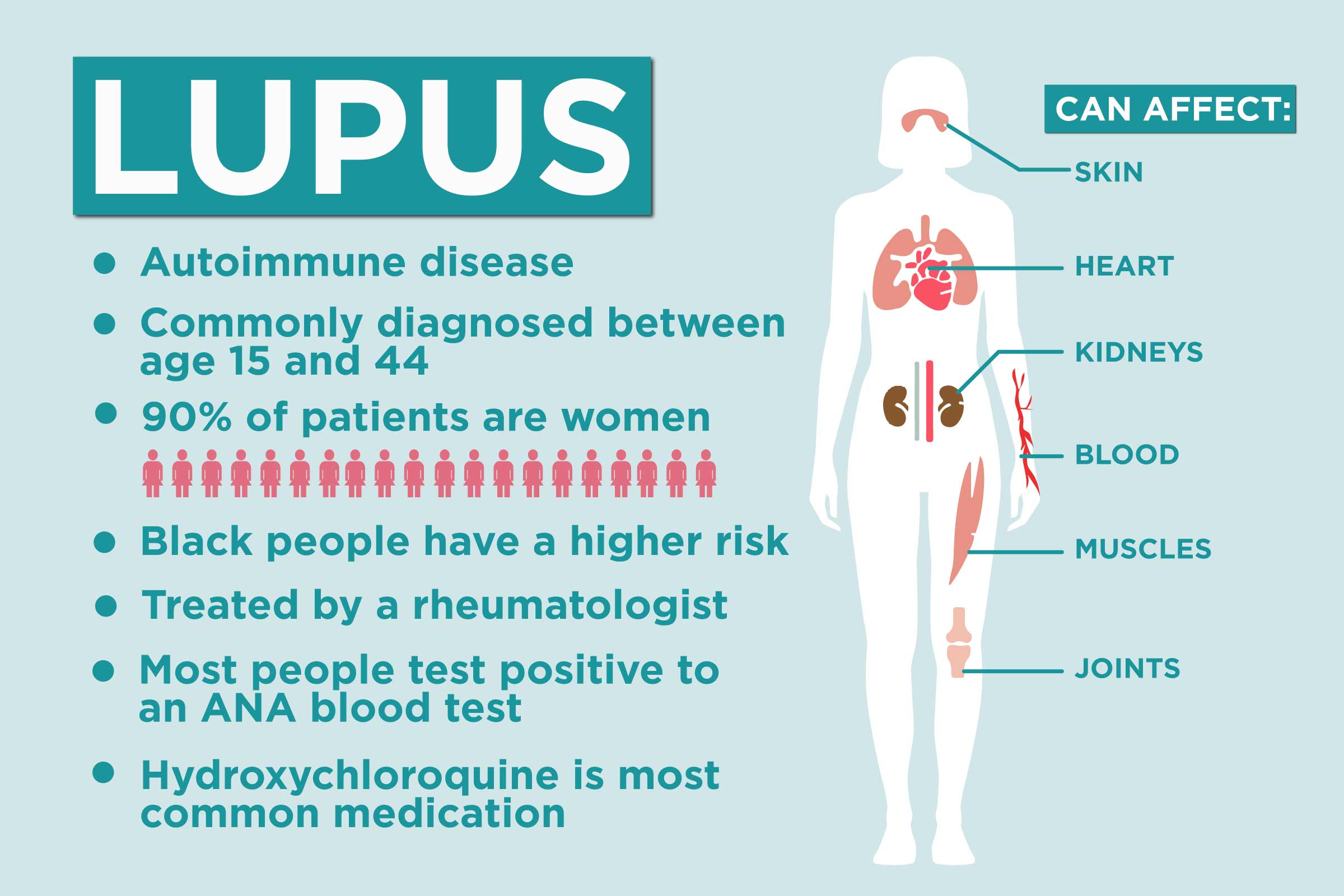
Lupus is an autoimmune disease where your body's defense system loses its mind and starts shooting at your own healthy tissue. It’s friendly fire. When people ask if you can die from lupus, they are usually asking about organ failure.
The biggest threat is usually Lupus Nephritis. About 40% of people with SLE develop kidney involvement. If your kidneys stop filtering waste because they are under constant attack from inflammation, you face end-stage renal disease. According to data from the Lupus Foundation of America, kidney failure is one of the leading causes of death among lupus patients. It’s sneaky. You might not feel your kidneys failing until the damage is significant, which is why rheumatologists are so obsessed with your urine samples.
Cardiovascular Risks Are the Silent Player
If you survive the early years of diagnosis without major organ involvement, the long-term threat actually shifts. It becomes about your heart. Chronic inflammation isn't just a joints-and-skin problem; it wreaks havoc on your blood vessels. People with lupus are much more likely to develop atherosclerosis (hardening of the arteries) at a young age.
We’ve seen cases where women in their 30s with lupus have heart attacks that you’d normally expect in an 80-year-old. It's wild. The inflammation accelerates the buildup of plaque. So, technically, the cause of death on a certificate might say "heart attack," but the underlying culprit was the lupus-driven inflammation that's been simmering for a decade.
👉 See also: Why Your Best Kefir Fruit Smoothie Recipe Probably Needs More Fat
The Infection Paradox
This is the part that feels like a cruel joke. To keep the lupus from killing you, doctors have to suppress your immune system. You take things like Prednisone, CellCept, or Methotrexate. These drugs are lifesavers. They stop the "friendly fire."
However, they also leave the door wide open for outside invaders.
Infections are actually a top cause of death for people living with SLE. A simple "flu" or a urinary tract infection can turn into sepsis incredibly fast because your body’s guards are essentially tied up or asleep on the job. It's a delicate balancing act. You need the meds to save your kidneys, but the meds make a common cold potentially dangerous. It requires a level of hyper-vigilance that is, frankly, exhausting.
Why Some People Face Higher Risks
The statistics aren't the same for everyone. It’s unfair, but it’s the reality of the clinical data. Mortality rates for lupus are significantly higher among women of color—specifically Black, Hispanic, and Native American women.
Studies, including those published in Arthritis & Rheumatology, show that Black patients often develop lupus at a younger age and experience more severe organ complications, particularly kidney issues. This isn't just about genetics; it's a messy overlap of biology, socioeconomic barriers to early diagnosis, and the quality of long-term care. If you catch lupus early, you can usually stay ahead of it. If it’s diagnosed after your kidneys are already scarred, the math changes.
✨ Don't miss: Exercises to Get Big Boobs: What Actually Works and the Anatomy Most People Ignore
Neuropsychiatric Lupus: The Brain Under Fire
Sometimes lupus crosses the blood-brain barrier. This is called Neuropsychiatric Lupus (NPSLE). It can cause seizures, strokes, or even "lupus psychosis." While less common than kidney issues, a severe neurological event can be fatal. It’s one of the most difficult manifestations to treat because it’s so hard to distinguish "lupus brain fog" from actual, structural damage or inflammation in the central nervous system.
Doctors look for signs like:
- Sudden, severe personality changes.
- New-onset seizures.
- Aseptic meningitis (inflammation of the brain lining not caused by bacteria).
- Transverse myelitis (inflammation of the spinal cord).
If you have these, it's an emergency. Full stop.
Can You Die From Lupus? Modern Survival Realities
We have to talk about the "Lupus Flare." Most of the time, a flare means you stay in bed for three days and your joints ache. But a "catastrophic" flare—though rare—can cause multiple organ systems to fail at once. This is often referred to as Catastrophic Antiphospholipid Syndrome (CAPS) in patients who carry certain antibodies. It involves small blood clots forming all over the body. It’s a medical crisis.
But I want to bring this back to earth. Most people with lupus do not die from it. They die with it.
🔗 Read more: Products With Red 40: What Most People Get Wrong
You live a life of managing symptoms. You learn to navigate the sun (which triggers flares), the meds, and the fatigue. You become an expert in your own bloodwork. The goal of modern medicine isn't just to keep you alive; it's to keep you in "remission" or "low disease activity." When the disease is quiet, your risk of dying from it drops to nearly the same level as someone without the condition.
Misconceptions That Scare People
People see "lupus" and think of the TV show House, where it’s the mysterious killer of the week. Or they see celebrities like Selena Gomez getting a kidney transplant and think that's the inevitable end-point for everyone. It's not.
- The "Everything is Lupus" Myth: Not every ache is a sign you're dying. You can still get a normal cold or have a normal backache.
- The "Pregnancy is Impossible" Myth: It used to be that doctors told women with lupus never to get pregnant because it could kill them. Today, with "high-risk" OBGYN care and careful timing (waiting until the disease is quiet for 6 months), most women have successful, healthy pregnancies.
- The "Chemo" Confusion: Some lupus drugs (like Cytoxan) are also used for cancer. This leads people to think lupus is a form of cancer. It’s not. It’s an autoimmune disease. The drugs are used because they are great at nuking overactive cells, whether they are cancerous or just confused immune cells.
Real Actions to Lower the Risk
If you’re living with this, or someone you love is, there are non-negotiable steps to take. This isn't just "lifestyle advice"; it's survival strategy.
- Sun Protection is Medicine: UV rays don't just give you a rash; they can trigger internal organ flares. Wear the SPF 50. Wear the hat. Even in the car.
- The Kidney Check: If your doctor doesn't ask for a urine sample at every visit, find a new doctor. Protein in the urine is the first warning sign of kidney trouble, and it's often reversible if caught early.
- Cardiovascular Health: Because lupus puts your heart at risk, you have to be boringly healthy. Watch your cholesterol. Keep your blood pressure low. Don't smoke. Smoking with lupus is like throwing gasoline on a fire; it makes the meds less effective and the vascular damage worse.
- Mental Health: There is a documented link between high stress and flares. Plus, the mortality rate is higher for those who lack a support system or suffer from untreated depression, which can lead to "non-adherence" (stopping your meds because you feel hopeless).
- Dental Hygiene: This sounds weird, right? But gum disease is a source of chronic inflammation and a gateway for bacteria. In an immunocompromised body, a mouth infection can turn into a heart infection (endocarditis).
What to Do Next
If you are worried about the life-expectancy of someone with lupus, the best thing you can do is focus on "Treat to Target." This is a medical strategy where you and your rheumatologist set a goal for zero symptoms and keep adjusting medications until you get there.
Don't settle for "I feel okay for having lupus." Aim for "I feel normal."
Schedule a baseline cardiovascular screening. Ask for a referral to a cardiologist who understands autoimmune triggers. Check your Vitamin D levels, as they are often bottomed-out in lupus patients and play a huge role in immune regulation. Most importantly, keep a log of symptoms. Lupus is a "liar"—it comes and goes. When you're in the doctor's office feeling fine, you'll forget that two weeks ago you couldn't breathe deeply or your ankles were swollen. Write it down. That data is what keeps you on the right side of the survival statistics.
Lupus is a serious, life-altering disease. But for the vast majority of people today, it is a chronic condition you live with, not a terminal one you die from.