Biology is messy. We’re taught in grade school that it’s a binary—XX or XY, boy or girl, blue or pink. But nature doesn't always follow the lesson plan. If you’ve ever wondered, can you be born with both genitalia, the short answer is yes, though it’s rarely as simple as having two full, distinct sets of "plumbing." It’s a spectrum of development that doctors and scientists call intersex traits or Differences of Sex Development (DSD).
Think of it like a radio dial. Most people are tuned clearly to one station or the other. However, some folks land somewhere in the static between frequencies. They’re perfectly healthy, but their anatomy doesn’t fit the standard medical definitions of male or female.
What Does "Both" Actually Look Like?
When people ask if you can be born with both, they’re usually thinking of "true hermaphroditism"—a term that’s actually outdated and considered offensive by many in the community. The modern medical term is ovotesticular DSD. This is exceptionally rare. In these cases, a person might have both ovarian and testicular tissue. Sometimes this happens in the same organ, which doctors call an ovotestis.
It’s a wild biological fluke.
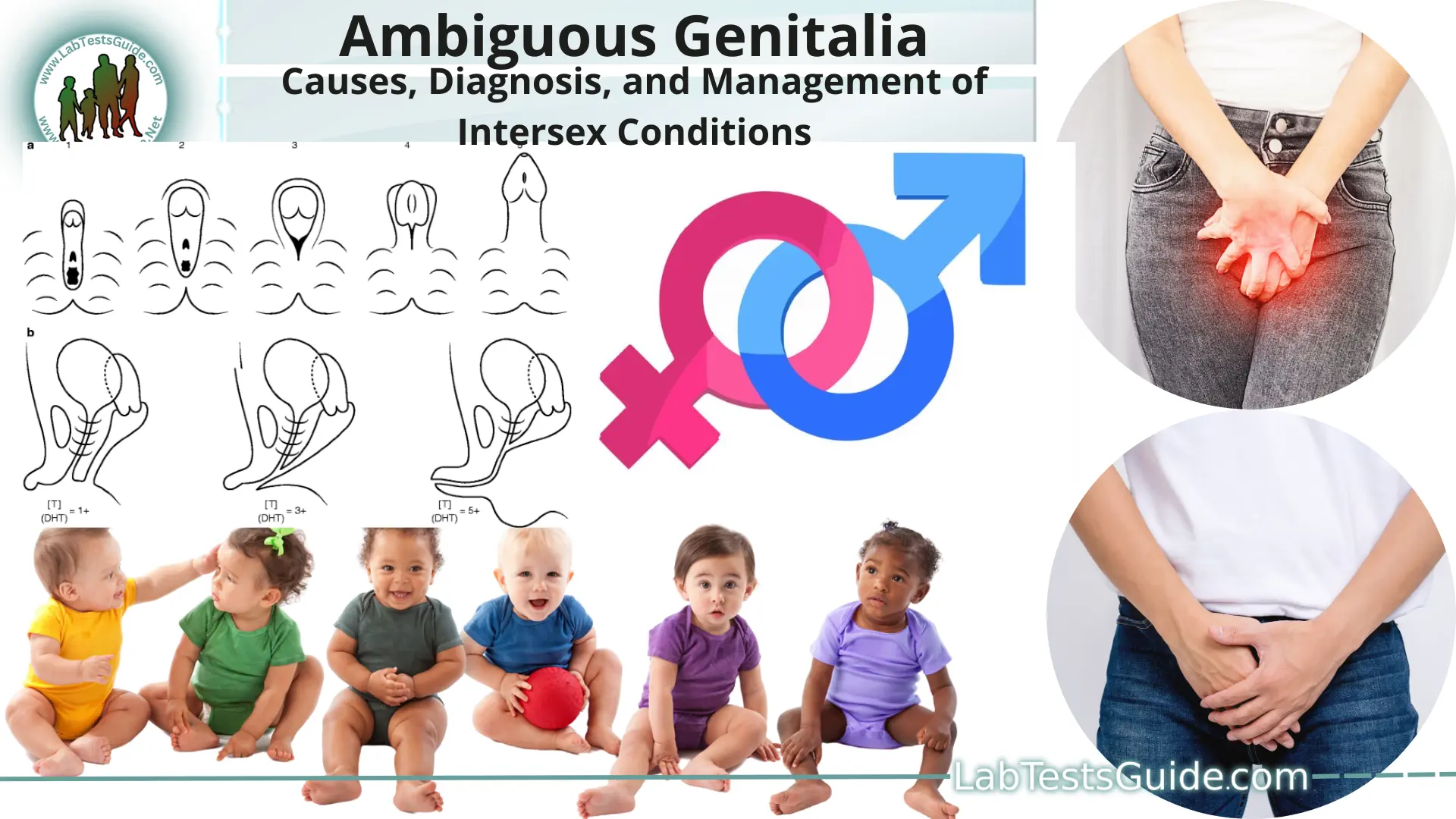
Most of the time, intersex traits show up as ambiguous genitalia. This means at birth, a baby’s anatomy might be hard to categorize. Maybe the clitoris is enlarged, or the penis is very small with an opening in a different spot (hypospadias). It’s not a "mistake." It’s just how the hormones and genetics shook out during those critical weeks in the womb.
Anne Fausto-Sterling, a professor at Brown University, has spent decades researching this. She famously suggested that sex is a continuum. While her "five sexes" theory from the 90s was more of a thought experiment, it highlighted a massive truth: humans are diverse.
The Role of Chromosomes and Hormones
We focus on what we can see, but the "both" part often happens under the skin. You might have someone who looks female on the outside but has XY chromosomes and internal testes. This is often called Androgen Insensitivity Syndrome (AIS).
Imagine your body has the "male" blueprint (XY), but the "locks" on your cells don't accept the "male" key (testosterone). The body just defaults to a female appearance. Often, people with AIS don't even know they have it until they hit puberty and don't start a period. They are often tall, have clear skin, and identify as women. They just happen to have a different internal setup.
👉 See also: Why Your Best Kefir Fruit Smoothie Recipe Probably Needs More Fat
Then there’s Congenital Adrenal Hyperplasia (CAH). This is a genetic condition where the adrenal glands pump out extra androgens. If an XX fetus has CAH, they might be born with an enlarged clitoris that looks very much like a penis.
Is it common?
Statistics are slippery. You’ll hear some activists say it’s as common as having red hair—about 1.7% of the population. Other researchers, like Leonard Sax, argue the number is much lower, closer to 0.018%, if you only count cases where the physical appearance is truly ambiguous.
Regardless of the decimal point, thousands of people are living with these variations right now. They’re your baristas, your mechanics, and your doctors.
The Controversy of "Corrective" Surgery
This is where things get heavy. For decades, the standard medical practice was to "fix" babies born with ambiguous genitalia. Doctors would perform surgery to make the child look more "normal" before they were even old enough to walk.
The logic was that it would save them from social stigma.
But here’s the kicker: many of these surgeries resulted in permanent nerve damage, loss of sexual sensation, or a gender identity that didn't match the surgery. Organizations like interACT (Advocates for Intersex Youth) have been fighting to stop these cosmetic procedures on infants. They argue that unless a surgery is life-saving—like making sure a child can urinate—it should wait until the person is old enough to decide for themselves.
In 2013, the United Nations even condemned these "normalizing" surgeries as a violation of human rights. It’s a massive shift in how the medical world views the question of "both" genitalia. We’re moving from a "fix it" mindset to an "accept it" mindset.
✨ Don't miss: Exercises to Get Big Boobs: What Actually Works and the Anatomy Most People Ignore
How Genetics Throw Curveballs
Biology loves a good twist. Take mosaicism, for example. This happens when a person has some cells with XX chromosomes and others with XY. It’s like a patchwork quilt. Depending on where those cells end up, the person’s internal and external anatomy can be a mix of both.
Then there’s 5-alpha reductase deficiency. In certain parts of the Dominican Republic, there’s a group of children known as "Guevedoces"—which literally translates to "penis at twelve."
They’re born looking like girls. They’re raised as girls. But when puberty hits, a massive surge of testosterone causes their bodies to change. They grow a penis and their testes descend. For them, having "both" or transitioning from one to another is just a part of the local culture. It’s a perfect example of how much of our "biological reality" is influenced by the hormones we’re bathing in before we’re even born.
Life as an Intersex Person
Honestly, if you were born with both or a mix of genitalia, the biggest challenge isn't the body itself. It’s the paperwork.
Our society is built on a binary. Driver's licenses, passports, bathroom signs, medical forms—they all want you to check a box. For someone whose body doesn't fit a box, that’s a daily headache.
Fortunately, things are changing. Several U.S. states and countries like Germany and Australia now allow an "X" gender marker. It’s a small change that makes a huge difference for someone who spent their whole life being told their body was a medical mystery that needed to be hidden.
Medical care is also evolving. Instead of "fixing" things, specialist teams at places like the Mayo Clinic or Johns Hopkins now include psychologists and ethicists. They focus on the long-term health and happiness of the kid, not just the aesthetics of their crotch.
🔗 Read more: Products With Red 40: What Most People Get Wrong
Common Myths That Need to Die
We need to clear the air on a few things.
First, being intersex is not the same as being transgender. A transgender person has a gender identity that differs from the sex they were assigned at birth. An intersex person has a physical body that doesn't fit the typical definitions of male or female. You can be both, but they are two different things.
Second, it’s not a "fetish." The adult film industry has spent years sensationalizing intersex bodies with derogatory slurs. In reality, this is a medical and biological variation. It’s about chromosomes, gonads, and hormones.
Third, intersex people are not "sterile" by default. While some variations do lead to infertility, many intersex individuals can and do have biological children. Every case is unique.
Moving Toward Understanding
If you or someone you know is navigating the reality of being born with both types of genital tissue or ambiguous features, the most important thing is to find a community. You aren't a "freak" or a medical anomaly. You’re a natural variation of the human species.
Actionable Insights for Navigating Intersex Realities:
- Seek Specialized Care: Don’t rely on a general practitioner who hasn't seen an intersex case since medical school. Look for DSD clinics at major university hospitals where they use a multidisciplinary approach.
- Wait on Surgery: Unless there is a clear medical necessity (like a blocked urethra), consensus is shifting toward waiting until the individual can provide informed consent for any cosmetic or gender-affirming procedures.
- Mental Health Matters: Finding a therapist who understands intersex issues is crucial. The trauma of early medical intervention or the stress of "passing" can be heavy.
- Check the Records: If you suspect you were born with ambiguous genitalia but your parents are vague about it, you have a right to your medical records. Knowing your specific diagnosis (like AIS or CAH) can help you manage your health as you age, especially regarding bone density and hormone balance.
- Connect with the Community: Groups like the Intersex Society of North America (archived but still relevant) and interACT provide resources that move beyond the clinical and into the human experience.
Biology doesn't always come in two neat packages. Sometimes, it comes in a beautiful, complex "both," and that’s perfectly okay. Understanding the science behind these variations helps strip away the stigma and lets us see the person, not just the anatomy.