You’re sitting on the couch, feeling weirdly wiped out, and suddenly your stomach starts doing somersaults. It isn’t food poisoning. You haven't had a stomach bug in years. But that nagging, queasy feeling won't quit. If you’re living with diabetes—or even if you aren’t—you might wonder: can hyperglycemia cause nausea? The short answer is a definitive yes. High blood sugar doesn't just mess with your energy; it can physically turn your stomach inside out.
It’s honestly one of the most frustrating symptoms because it’s so vague. Nausea can mean anything, right? But when your glucose levels climb too high, your body starts a chain reaction that hits the digestive system hard.
✨ Don't miss: Healthiest Instant Pot Recipes That Actually Taste Good
The Gut-Blood Sugar Connection
When your blood sugar spikes, your body isn't just "sweet." It's actually struggling. Normally, your body uses insulin to move sugar from your blood into your cells for energy. Without enough insulin—or if your body can't use it right—that sugar just sits there. It's like a traffic jam in your veins.
The most direct reason high blood sugar makes you feel like throwing up is gastroparesis. This is basically a fancy medical term for "paralyzed stomach." Over time, chronic hyperglycemia damages the vagus nerve. That's the nerve responsible for telling your stomach muscles to contract and move food along to the small intestine. When that nerve gets fried by high sugar levels, food just sits in your stomach. It rots. It ferments. And yeah, it makes you feel incredibly nauseous.
But it’s not always about long-term damage. Even a sudden, sharp spike can cause acute nausea. When your kidneys try to flush out the excess sugar, you pee more. You get dehydrated. Dehydration by itself is enough to make anyone feel green around the gills.
When Nausea Becomes a Warning Sign: DKA
We need to talk about the scary stuff for a second. If you have Type 1 diabetes (and sometimes Type 2), nausea isn't just an annoyance—it can be a red flag for Diabetic Ketoacidosis (DKA).
Think of DKA as a metabolic emergency. Since your cells can't get sugar for fuel, they start burning fat way too fast. This produces ketones. Ketones are acidic. When they build up in your blood, they literally poison your system.
Nausea is often the very first sign of DKA. If that nausea is paired with stomach pain, a fruity smell on your breath, or deep, rapid breathing (Kussmaul breathing), you’re in trouble. This isn't a "wait and see" situation. You need a hospital. According to the American Diabetes Association, DKA is life-threatening if ignored. It's not just a stomach ache; it's your blood turning into acid.
Why Does My Stomach Hurt After I Eat?
You’d think eating would make you feel better, but with hyperglycemia, it's often the opposite. High glucose slows down gastric emptying.
Imagine your stomach is a funnel. Usually, it pours food through at a steady rate. Hyperglycemia puts a cap on that funnel. You eat a normal meal, but your stomach can’t dump it. You feel full after three bites. You feel bloated. You feel like you're going to gag.
- Early Satiety: Feeling stuffed after a tiny snack.
- Reflux: Food backing up because it has nowhere else to go.
- Vomiting: Your body’s "emergency exit" when the "normal exit" is blocked.
Many people mistake this for a simple case of indigestion or GERD. They pop some Tums and move on. But if the underlying cause is high blood sugar, the Tums won't do a lick of good. You’ve got to bring those numbers down to get the "funnel" moving again.
The Role of Dehydration and Electrolytes
Hyperglycemia is a thirsty condition. Your body is desperate to dilute the sugar in your blood. It pulls water from your tissues, sends it to your kidneys, and you spend half your day in the bathroom.
This leads to a massive imbalance in electrolytes like magnesium, potassium, and sodium. Your digestive tract needs these minerals to function. When they're out of whack, the smooth muscles in your gut don't fire correctly.
It's a vicious cycle. You're nauseous because your sugar is high. You're dehydrated because your sugar is high. The dehydration makes the nausea worse. You don't want to drink water because you feel sick. Your sugar stays high because you're dehydrated. It’s a mess.
Is It Your Medication?
Wait. Sometimes it's not the sugar itself, but the stuff we take to control it.
If you’ve recently started Metformin, you know exactly what I’m talking about. Metformin is notorious for "the runs" and intense nausea during the first few weeks. Similarly, GLP-1 agonists like Ozempic (semaglutide) or Mounjaro (tirzepatide) work specifically by slowing down your digestion. That’s how they help you lose weight and control sugar—they make you feel full longer.
But sometimes they slow things down too much.
If you're asking "can hyperglycemia cause nausea," you also have to ask if your meds are mimicking the feeling. You might have perfectly controlled sugar but feel like garbage because your body is reacting to the dose. It's a delicate balance. Always talk to your endocrinologist before you decide to just stop taking something, though. Sudden stops can lead to the very sugar spikes you're trying to avoid.
How to Manage the "Sugar Sickness"
So, you’re feeling sick and your CGM or finger-stick confirms you're high. What now?
First, check for ketones. If you're over 240 mg/dL, use a ketone strip. If they're "large" or "high," stop reading this and call a doctor.
If ketones are low or negative, focus on hydration. Sip—don't chug—water. Chugging will just make you vomit. Try clear broths or sugar-free electrolyte drinks.
Movement helps, but only if your sugar isn't too high. A gentle walk can help insulin sensitivity, but if you're in the 300+ range, heavy exercise can actually push your sugar higher because of the stress response. Keep it easy.
Real-World Strategy:
- Small, Frequent Sips: Water is your best friend.
- Check the Clock: If you haven't been able to keep liquids down for 4 hours, it's time for the ER.
- Cool Compresses: Sometimes the sensory distraction of a cold towel on the neck can settle the "brain" part of nausea while you wait for your insulin to work.
- Ginger: Some swear by it, but make sure it’s sugar-free ginger tea, not sugary ginger ale.
The Myth of the "Quick Fix"
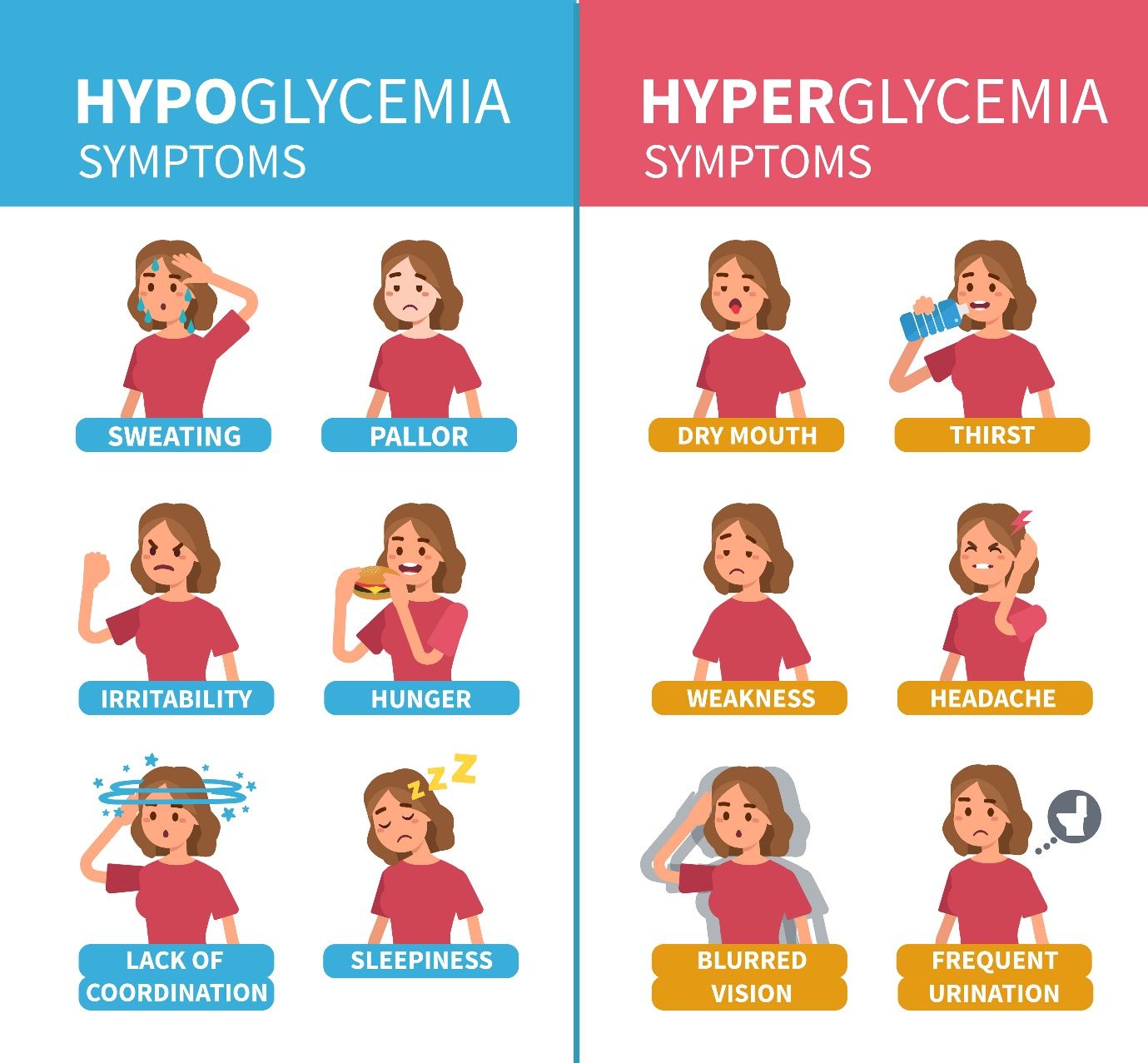
A lot of people think they can just "eat through" the nausea with crackers. If your nausea is from low blood sugar (hypoglycemia), crackers are great. But if it's from high blood sugar, more carbs are the last thing you need.
You have to know your numbers. Treating a high like a low will make you feel infinitely worse.
Hyperglycemia-induced nausea is basically your body’s check engine light. It’s telling you that the internal chemistry is skewed. Don't ignore it. If you find yourself consistently nauseous in the mornings or after meals, it’s a sign that your current management plan isn't cutting it. Maybe your basal insulin is too low, or your carb-to-insulin ratio is off.
Actionable Steps to Take Right Now
- Test Immediately: Don't guess. Use your meter. If you're above your target range, follow your doctor's correction bolus protocol.
- Ketone Check: If you're Type 1 or insulin-dependent Type 2, test your urine or blood for ketones.
- Hydrate with Precision: Drink 8 ounces of water every hour, taken in small sips.
- Log the Trigger: Did you eat a high-fat meal? Stress out at work? This helps identify if it's a "spike" nausea or a "slow digestion" (gastroparesis) nausea.
- Review Medications: Look at when you took your last dose of Metformin or your GLP-1 injection.
- Contact Your Team: If the nausea persists for more than 24 hours even after sugar levels return to normal, you need a gastric emptying study to check for nerve damage.
Hyperglycemia and nausea are tightly linked through a complex web of nerve signaling, hydration levels, and chemical balances. While it's a common symptom, it's never one you should "just live with." Consistent nausea is usually a signal that your A1c is trending in the wrong direction or that your gut is starting to pay the price for high glucose. Address the sugar, and the stomach usually follows suit.
Next Steps for Long-Term Relief
- Audit your nighttime glucose: Morning nausea is often a result of "Dawn Phenomenon" or high overnight readings.
- Request a Gastroparesis Screen: If you feel full quickly even when sugars are normal, ask your doctor for a "4-hour egg scan" (scintigraphy).
- Adjust Fiber Intake: While fiber is usually good, if your gut is slowed down by hyperglycemia, too much raw fiber can actually cause a "blockage" (bezoar) that increases nausea.
- Track Patterns: Use an app to note when the nausea hits. Is it 30 minutes after a meal or 3 hours? This data is gold for your doctor.