If you’ve ever sat in a psychiatrist’s office feeling like your brain is made of lead, you've probably heard of Wellbutrin. It’s the brand name for bupropion. For people with standard depression, it’s often a godsend because it doesn’t cause the weight gain or the "zombie" sexual side effects that usually come with SSRIs like Prozac or Zoloft. But when we talk about bupropion and bipolar disorder, the conversation gets a lot more complicated, and honestly, a little bit risky.
It’s a tightrope walk. You’re depressed. You can't get out of bed. You need a lift. But in bipolar disorder, if you lift the mood too much, you don't just hit "normal"—you blast right past it into mania.
The "Happy-Horny-Skinny" Pill and the Bipolar Brain
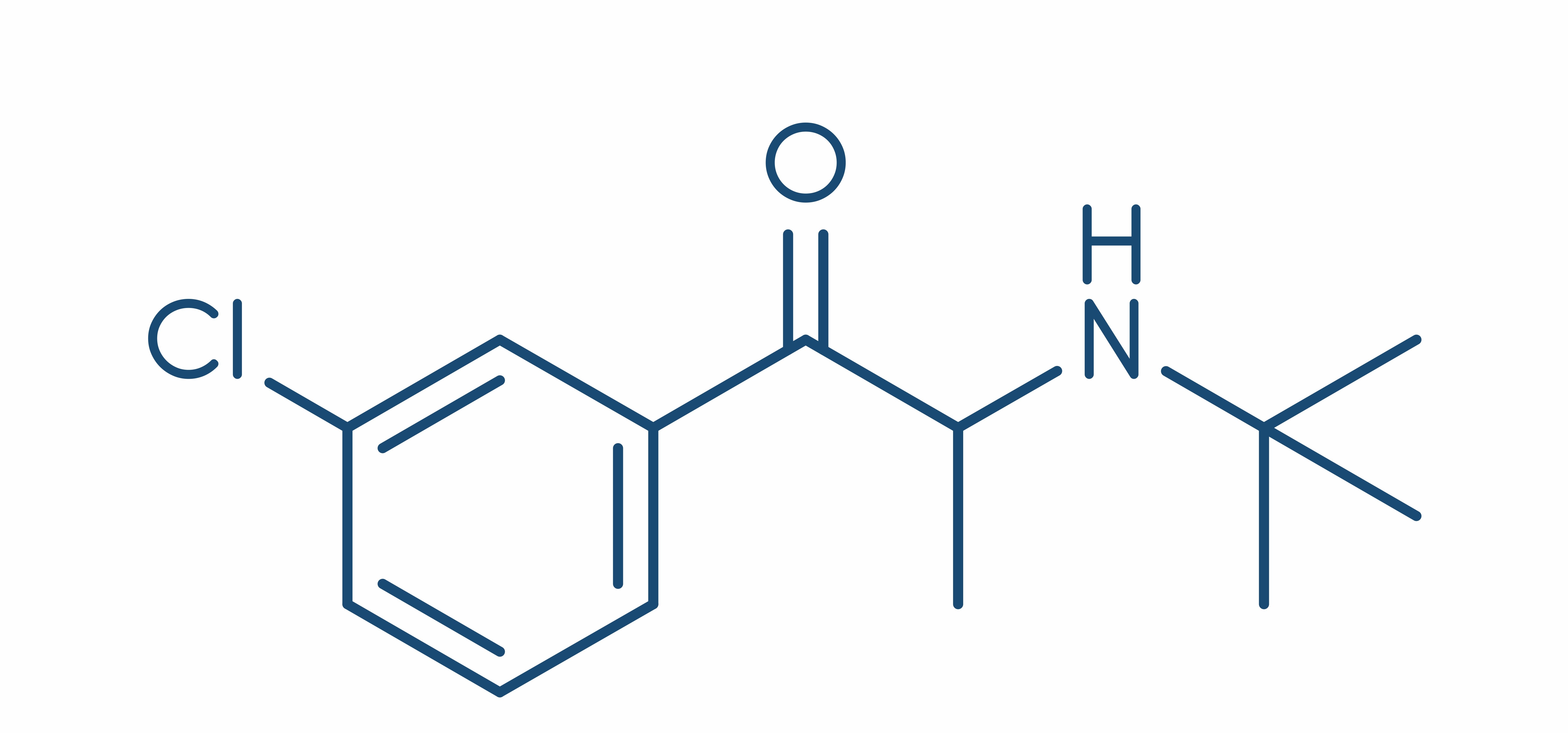
Doctors sometimes jokingly call bupropion the "happy-horny-skinny" pill. It sounds like a marketing dream. Unlike most antidepressants that mess with serotonin, bupropion targets norepinephrine and dopamine. It’s a NDRI (Norepinephrine-Dopamine Reuptake Inhibitor). This matters because dopamine is the brain's reward chemical. It gives you "get up and go."
But here is the catch.
In a bipolar brain, dopamine is already a volatile substance. Think of it like pouring gasoline on a flickering fire. For some, it provides the perfect amount of warmth to break a depressive cycle. For others? It’s a total inferno. We are talking about the "switch." This is the clinical term for when an antidepressant triggers a manic or hypomanic episode.
The medical community used to be terrified of using any antidepressant for bipolar disorder. The fear was that every patient would immediately spiral into psychosis or start spending their life savings on a whim. Newer research, specifically large-scale reviews like those found in the Journal of Clinical Psychiatry, suggests bupropion might actually have a lower "switch rate" than older tricyclic antidepressants or even some SSRIs. But "lower" isn't "zero."
Why Bupropion is Different (and Sometimes Dangerous)
Most people think all antidepressants are basically the same. They aren't. Not even close. If you take a drug like Effexor (an SNRI), you are hitting the serotonin and norepinephrine systems hard. Those are notorious for causing rapid cycling in bipolar patients.
👉 See also: My eye keeps twitching for days: When to ignore it and when to actually worry
Bupropion stays away from serotonin.
Because it acts more like a very mild stimulant—it’s actually chemically related to cathinones—it addresses the "sluggish" symptoms of bipolar depression better than most. If you have bipolar II, where you mostly deal with soul-crushing lows and only occasional "up" periods of high productivity, your doctor might be more willing to try it.
The Anxiety Factor
There is a side effect of bupropion that doesn't get talked about enough in the context of bipolar disorder: the "jitters."
Because it increases norepinephrine (your body's adrenaline cousin), it can make you feel incredibly "wired." If you already have a tendency toward mixed episodes—where you feel depressed and agitated at the exact same time—bupropion can make you feel like you want to crawl out of your skin. It’s not a fun feeling. It’s that vibrating, heart-racing anxiety that makes you feel like something bad is about to happen.
What the Data Actually Says
Let's look at the STEP-BD study (Systematic Treatment Enhancement Program for Bipolar Disorder). This was a massive, landmark study. It found that for many people, adding an antidepressant to a mood stabilizer didn't actually provide a huge benefit over the mood stabilizer alone.
Wait.
✨ Don't miss: Ingestion of hydrogen peroxide: Why a common household hack is actually dangerous
That sounds discouraging, right? If it doesn't help more than a mood stabilizer, why take the risk? Well, because "average" data doesn't account for individuals. Some people are "antidepressant responders." They are the ones whose biology specifically needs that dopamine kick.
The Mood Stabilizer Rule
If you are looking into bupropion and bipolar disorder, there is one non-negotiable rule most experts, like those at the Mayo Clinic or Johns Hopkins, agree on: Never take it alone.
Taking bupropion without a "buffer"—like Lithium, Lamictal (lamotrigine), or an atypical antipsychotic—is like driving a car with an accelerator but no brakes. You might go fast, but you aren't going to be able to stop when the curve in the road (mania) comes up.
Real-World Nuance: The Risk of "Mixed States"
One of the biggest misconceptions is that mania is always "happy." It’s not. Sometimes mania is just pure, unadulterated rage. Or it's a "mixed state" where you have the energy of mania but the hopelessness of depression.
This is where bupropion gets tricky.
If you start feeling like you don’t need to sleep, or if you’re suddenly starting five new business ventures at 3:00 AM, the drug is likely pushing you into a manic "switch." But if you just feel incredibly irritable and snappy at your spouse, you might be in a mixed state triggered by the norepinephrine boost.
🔗 Read more: Why the EMS 20/20 Podcast is the Best Training You’re Not Getting in School
The Seizure Threshold: A Specific Warning
I have to mention this because it’s a specific quirk of bupropion. At higher doses, it can lower the seizure threshold. This is rare, but it's why doctors are very careful about the dosage, especially if you have a history of eating disorders (like bulimia) or alcohol withdrawal. For a bipolar patient who might already be on a cocktail of medications, adding a drug that affects the seizure threshold requires a very careful balancing act by a psychiatrist.
How to Manage the Risks
If you and your doctor decide that bupropion is the right move for your bipolar depression, you have to be a detective of your own mind. You can't just take the pill and forget about it.
First, track your sleep. Sleep is the "canary in the coal mine" for bipolar disorder. If you notice you’re sleeping three hours a night and feeling totally refreshed, that’s a red flag. The bupropion is doing too much.
Second, watch for the "honeymoon." Sometimes people feel amazing the first week on bupropion because of that initial dopamine hit. But the real therapeutic effect takes 4 to 6 weeks. If you feel "cured" on day three, tell your doctor. That’s usually a sign of an impending switch, not a miracle cure.
Third, be honest about your caffeine intake. Since bupropion is already stimulating, that third cup of coffee might be the thing that pushes you into a panic attack or a hypomanic state.
Actionable Steps for Navigating This Treatment
It’s easy to get overwhelmed by the "what ifs" of medication. If you're considering this path, here is how to handle it practically.
- Establish a baseline first. Do not start bupropion during a period of instability. Make sure your mood stabilizer (Lithium, Valproate, etc.) is at a therapeutic level in your bloodstream before adding an antidepressant.
- Request the XL (Extended Release) version. The IR (Immediate Release) version creates a "spike" in the blood that is much more likely to trigger anxiety or mania. The XL version releases slowly over 24 hours, which is generally much smoother for a bipolar brain.
- Keep a daily mood log. Use an app like Daylio or a simple paper journal. Mark your mood from 1 to 10 and, more importantly, track your "energy" levels. High energy with a low mood is a dangerous combination.
- Have a "Rescue Plan." Talk to your doctor before you start. Ask: "If I start feeling manic on this, what do I do?" Usually, the answer is to stop the bupropion immediately and possibly increase your mood stabilizer, but you need that plan in writing.
- Monitor your weight and habits. While bupropion is "weight-neutral," if you find you are losing weight too fast because you "forget to eat," that can trigger physical stress that worsens bipolar cycling.
The reality of bupropion and bipolar disorder is that it is a tool. In the right hands, with the right "buffer" medications, it can pull someone out of the darkest, most stagnant depression they’ve ever experienced. But it isn't a "set it and forget it" medication. It requires a partnership between you and a doctor who understands that your brain doesn't react to antidepressants the way a "typical" brain does.
Always prioritize stability over a "high." The goal isn't to be ecstatic; it's to be functional, steady, and capable of experiencing life without the crushing weight of the lows or the destructive fire of the highs.