You’re sitting in that crinkly paper-covered chair at the doctor's office. The cuff tightens. It squeezes until your pulse thumps in your ears, then slowly deflates. The nurse mutters something like "124 over 82" and scribbles it down. Most of us just nod. We know lower is usually better, but honestly, if you asked the average person to explain blood pressure systolic over diastolic without using a medical textbook, they’d probably stumble. It’s just two numbers separated by a slash, right? Well, not exactly. Those numbers are a literal mechanical readout of how your heart is fighting against your pipes.
It’s about pressure. Specifically, the force of blood pushing against the walls of your arteries. If that pressure is too high for too long, things start to break. Not all at once, usually. It’s more like a slow-motion wear and tear that eventually leads to a catastrophic failure of the pump or the plumbing.
Understanding the top and bottom numbers
So, let's break it down. The top number is the systolic pressure. This is the big one. It measures the force your heart exerts on your artery walls every single time it beats. Think of it as the "active" phase. When that muscle contracts, it blasts blood out into the system. That’s the peak pressure.
The bottom number? That’s the diastolic pressure. This happens when your heart is resting between beats. It’s the "refilling" phase. Even though the heart isn't actively pushing, there’s still pressure in the system. It never drops to zero. If it did, you’d be in serious trouble. Basically, the diastolic number tells us how much resistance your blood vessels are offering when the heart is taking a millisecond-long nap.
Why do we care more about one than the other? For a long time, doctors focused heavily on the diastolic number, thinking it was the better predictor of heart attacks. But things changed. Current research, including major findings from the American Heart Association, suggests that for people over 50, the systolic number is actually the more important predictor of cardiovascular disease. As we age, our large arteries get stiff. They don't bounce back like they used to. This stiffness makes that top number climb.
The 120/80 myth and the new reality
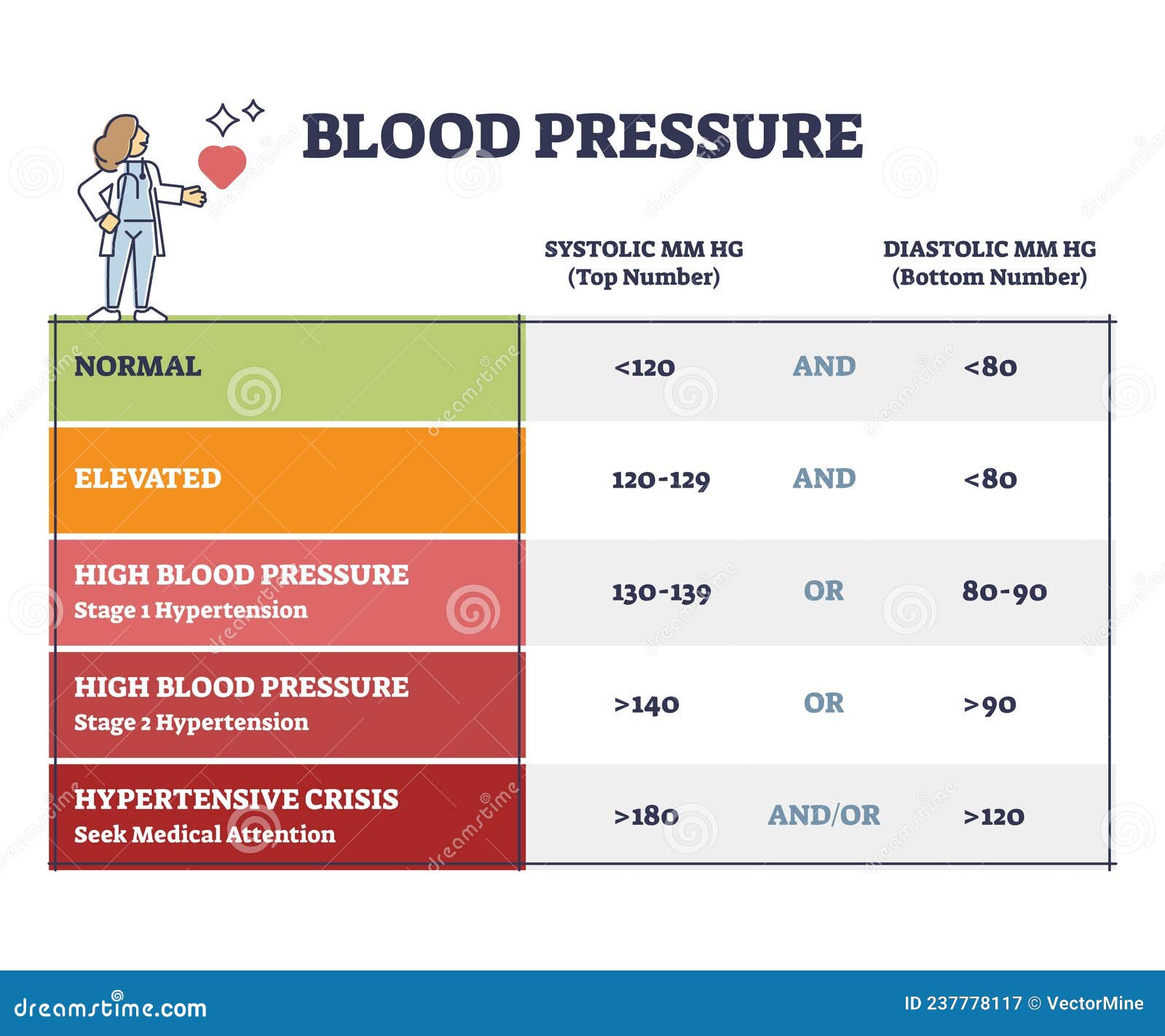
For decades, 120/80 was the gold standard. It was the "perfect" score. But medicine isn't static. In 2017, the American College of Cardiology and the American Heart Association shifted the goalposts. They didn't do it to sell more meds; they did it because the data showed that even "pre-hypertension" was causing strokes and heart failure.
📖 Related: How to Use Kegel Balls: What Most People Get Wrong About Pelvic Floor Training
Now, "Normal" is strictly less than 120/80 mmHg. If your blood pressure systolic over diastolic reads 121/81, you are technically in a different category. "Elevated" is when the top number is between 120-129 and the bottom is less than 80. Once you hit 130/80, you’ve officially entered Stage 1 Hypertension territory.
It feels a bit nitpicky, doesn't it? A few points here or there. But on a physiological level, that extra pressure is like running a garden hose at a higher PSI than it was rated for. Eventually, you get leaks. In the human body, those leaks are called strokes or aneurysms. Or the hose gets scarred and narrowed, which is how we get atherosclerosis.
When the gap between numbers gets weird
Most of the time, the two numbers move somewhat in tandem. If your systolic goes up, your diastolic usually follows. But sometimes they drift apart. This is called Pulse Pressure. If you have a systolic of 150 but a diastolic of 80, your pulse pressure is 70. A wide pulse pressure—anything over 60—is often a red flag for stiff arteries or even heart valve issues like aortic regurgitation.
Then there’s "Isolated Systolic Hypertension." This is super common in older adults. The top number is high, but the bottom number is perfectly fine or even low. It’s a tricky situation for doctors because lowering the top number might push the bottom number too low, making the patient feel dizzy or faint. It’s a delicate balancing act that requires more than just a standard prescription.
The "White Coat" effect and why one reading is useless
Never trust a single reading. Seriously. Your blood pressure is a moving target. It changes when you talk, when you cross your legs, if your bladder is full, or if you’re stressed about being at the doctor’s office. That last one is "White Coat Hypertension." Your brain sees the stethoscope and triggers a fight-or-flight response, sending your numbers into the stratosphere.
👉 See also: Fruits that are good to lose weight: What you’re actually missing
On the flip side, there’s "Masked Hypertension." This is actually scarier. Your pressure looks fine at the clinic, but it’s dangerously high when you’re at home or work. This is why many cardiologists now insist on home monitoring. You need a "trend," not a "snapshot." If you take your blood pressure every morning for a week and the average is 135/85, that’s way more informative than a one-time 118/78 at the pharmacy kiosk.
Specific factors that mess with your stats
It's not just about salt. While sodium is a huge factor—it makes your body hold onto water, which increases the volume of blood the heart has to pump—it's only part of the puzzle. Potassium is arguably just as important. Think of potassium as the "anti-sodium." It helps ease the tension in your blood vessel walls. If you’re low on potassium, your vessels stay constricted, and your blood pressure systolic over diastolic stays high.
Sleep apnea is another silent killer of your numbers. If you stop breathing at night, your oxygen levels drop. Your brain panics. It sends a surge of adrenaline to wake you up. This spikes your blood pressure in the middle of the night. If this happens 30 times an hour, your system never gets the "nocturnal dip" it needs. Normally, your blood pressure should drop by 10% to 20% while you sleep. If it doesn't, you're at a much higher risk for a cardiac event.
Practical steps to take right now
Managing these numbers isn't always about starting a heavy regimen of ACE inhibitors or beta-blockers, though those are literal lifesavers for millions. Often, the most profound changes come from things that sound boring but are actually incredibly effective.
First, get a validated home cuff. Don't buy the cheapest one on the shelf. Look for one that is clinically validated, often marked with a "dabl" or "ESH" seal. Sit quietly for five minutes before you hit the button. No phone. No TV. Just sit. Feet flat on the floor.
✨ Don't miss: Resistance Bands Workout: Why Your Gym Memberships Are Feeling Extra Expensive Lately
Second, look at your "input." The DASH diet (Dietary Approaches to Stop Hypertension) is the gold standard here. It focuses on fruits, veggies, and lean protein, but specifically pushes for high potassium, calcium, and magnesium. It’s been shown in studies to lower systolic pressure by 8 to 14 points. That’s as effective as some medications.
Third, move. You don't have to run marathons. Even 150 minutes of moderate exercise a week—like brisk walking—makes your heart a more efficient pump. A stronger heart can push more blood with less effort, which naturally lowers the force on your arteries.
Realities of medication and long-term health
If your doctor does suggest medication, don't view it as a failure. For many, hypertension is genetic. You could be a vegan marathon runner and still have a systolic of 145 because your kidneys or your arteries are just wired that way. The goal isn't "no meds," the goal is "no stroke."
Modern medications are highly nuanced. Thiazide diuretics help the kidneys flush out salt. Calcium channel blockers relax the muscles in your blood vessel walls. ARBs (Angiotensin II Receptor Blockers) prevent a specific hormone from narrowing your vessels. Sometimes a "low-dose combo" of two different meds works better and has fewer side effects than a high dose of just one.
Immediate Actionable Strategy
- Verify your baseline. Take your blood pressure twice a day (morning and evening) for seven days. Ignore the first day's readings and average the rest.
- The "Salt Swap." Don't just stop salting your food; start checking labels for "hidden" sodium in bread, sauces, and frozen meals. Aim for under 1,500mg a day if your numbers are high.
- The 5-Minute Decompression. If your systolic is creeping up due to stress, practice "box breathing"—inhale for 4, hold for 4, exhale for 4, hold for 4. It can acutely lower your pressure by calming the autonomic nervous system.
- Check your waistline. For every kilogram (about 2.2 pounds) of weight you lose, your systolic pressure can drop by about 1 mmHg. It’s one of the most direct correlations in medicine.
- Monitor your "dippers" status. If you can, use a monitor that tracks you while you sleep once in a while. If your blood pressure doesn't drop at night, talk to your doctor about a sleep study or changing the time of day you take your medication.