You finally get the news from your doctor: your blood pressure is high. It’s a "silent killer," they say. You take the script, you go to the pharmacy, and you start the pills because you want to live a long time. Then, a few weeks later, something else stops working. It's frustrating. It's embarrassing. And honestly, it’s one of the biggest reasons men stop taking their life-saving medication without telling their doctors.
The link between blood pressure meds and ed isn't just in your head. It’s a biological reality. But here’s the kicker—high blood pressure itself is actually the primary cause of erectile dysfunction, not always the pills. Hypertension damages the lining of your blood vessels. When those vessels can't dilate properly, blood can't flow where it needs to go when the moment strikes. You’re caught in a "damned if you do, damned if you don't" cycle.
But it doesn't have to be that way.
The Culprits: Which Meds Are the Worst Offenders?
Not all blood pressure drugs are created equal when it comes to your sex life. Some are notorious for causing issues, while others are actually "neutral" or might even help.
Diuretics (water pills) are often the first line of defense for doctors. Hydrochlorothiazide, or HCTZ, is a classic example. These drugs help your body get rid of excess salt and water. Unfortunately, they also decrease the force of blood flow into the penis and can deplete your body of zinc, which is necessary to produce testosterone. If you're on a diuretic and notice a sudden drop-off in performance, there’s a direct link there.
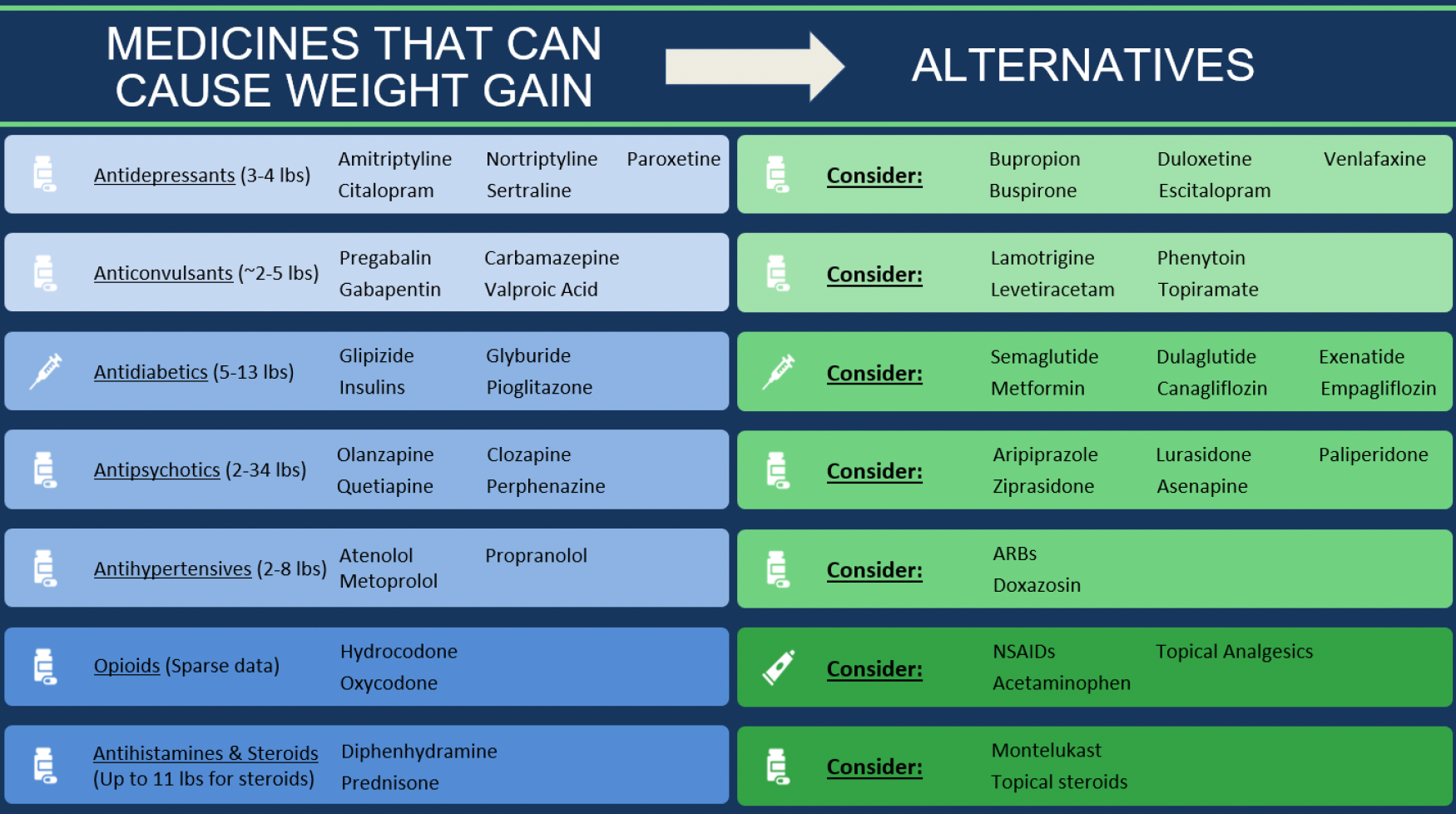
Then you have the Beta-blockers. Drugs like Atenolol or Metoprolol work by slowing your heart rate and reducing the force of contraction. That’s great for your heart, but not great for an erection, which relies on a nervous system that’s "ready to go." Beta-blockers can dampen the nerve impulses that lead to an erection. They can also make you feel a bit lethargic or depressed, which is a total libido killer.
- Propranolol is one of the older ones often cited in studies for having a higher incidence of sexual side effects.
- Interestingly, newer beta-blockers like Nebivolol (Bystolic) work differently. They actually stimulate the release of nitric oxide, which helps blood vessels relax and open up.
If you're on an older beta-blocker and struggling, it's worth asking about a switch.
🔗 Read more: Why Doing Leg Lifts on a Pull Up Bar is Harder Than You Think
Why Your Doctor Might Have Missed the Mark
Doctors are busy. Sometimes they focus so much on the "numbers" (getting that BP below 120/80) that they forget to ask about the quality of life stuff.
Research published in the Journal of the American Geriatrics Society has shown that many patients won't bring up sexual dysfunction unless the provider asks first. And most providers don't ask. They assume if you don't say anything, everything is fine. Meanwhile, you’re sitting at home wondering if this is just what getting older feels like. It’s not.
The Good News: The "ED-Friendly" Options
If you’re dealing with blood pressure meds and ed, you need to know about ACE inhibitors and ARBs.
ACE inhibitors (like Lisinopril) and ARBs (like Losartan or Valsartan) are generally considered "sex-neutral." In some studies, ARBs like Losartan actually improved sexual function in men who previously had issues. Why? Because they block angiotensin II, a chemical that constricts blood vessels. By blocking it, they allow for better blood flow throughout the entire body, including the pelvic region.
Calcium channel blockers, such as Amlodipine, also tend to have a lower risk of causing ED compared to diuretics and beta-blockers. They work by relaxing the muscles of your blood vessels. While they aren't exactly "performance enhancers," they usually don't throw a wrench in the gears.
The Psychology of the "Placebo" Effect
We have to talk about the "nocebo" effect. It’s the opposite of a placebo.
💡 You might also like: Why That Reddit Blackhead on Nose That Won’t Pop Might Not Actually Be a Blackhead
A famous study published in European Urology took three groups of men starting on the beta-blocker Atenolol.
- Group one was not told the name of the drug or the side effects.
- Group two was told the name but not the side effects.
- Group three was told the name and specifically warned about ED.
The results were wild. Only 3% of the group who didn't know about the side effects reported ED. But nearly 32% of the group who was warned reported it.
The mind is a powerful thing. If you're stressed about your blood pressure and then you read a pamphlet saying your meds cause ED, your brain might create the very problem you're afraid of. Stress increases adrenaline, and adrenaline constricts blood vessels. It’s the biological "off switch" for an erection.
Can You Take ED Meds With BP Meds?
This is the $64,000 question. For most guys, the answer is yes, but with a massive, life-saving caveat.
NEVER take PDE5 inhibitors (Viagra, Cialis, Levitra) if you are taking nitrates for chest pain.
Nitrates and ED meds both dilate blood vessels. If you combine them, your blood pressure can drop to dangerous, even fatal, levels. However, if you are just on standard blood pressure meds like an ACE inhibitor or a calcium channel blocker, drugs like Sildenafil or Tadalafil are usually safe and effective. In fact, many cardiologists prescribe them specifically to help men stay compliant with their BP medications.
📖 Related: Egg Supplement Facts: Why Powdered Yolks Are Actually Taking Over
Real-World Nuance: It’s Rarely Just the Meds
Let’s be real for a second. If you have high blood pressure, you might also have:
- High cholesterol
- Type 2 Diabetes
- Extra weight around the middle
- High stress levels
All of these factors contribute to ED. It's easy to blame the pill you started last month, but the reality is often "vascular disease" in general. The arteries in the penis are much smaller (about 1-2mm) than the arteries in the heart (3-4mm). Often, ED is the "canary in the coal mine"—it’s the first sign that your cardiovascular system is struggling.
Practical Steps to Take Right Now
If you think your blood pressure meds and ed are linked, don't just stop taking your pills. A stroke is worse than a bad night in the bedroom. Do this instead:
- Track the Timeline: Did the issues start exactly when you started the new med? Or were they creeping up before? Be honest with yourself.
- Review Your Zinc Levels: Especially if you’re on a diuretic. A simple supplement might help if you're deficient.
- Ask for an ARB: If you’re on a beta-blocker or diuretic, ask your doctor, "Hey, can we try Losartan instead?" It’s often just as effective for BP and much better for your sex life.
- The "Weekend Holiday" is a Myth: Do not skip your BP meds on the weekend thinking it will help you perform. These drugs need a steady level in your blood to work, and skipping doses can cause dangerous "rebound" hypertension.
- Check Your Testosterone: High BP and low T often go hand-in-hand. It might not be the meds at all; it might be your hormone levels.
- Focus on Nitric Oxide Foods: Beets, leafy greens, and garlic help naturally boost nitric oxide, which supports what the meds are trying to do anyway.
Summary of Actionable Insights
If you are struggling, remember that you have options. Medicine is an art as much as a science. If one drug causes side effects, there are five others in a different class that might work perfectly without the "downstairs" drama.
- Switching Classes: Moving from a Thiazide diuretic to an ACE Inhibitor or ARB is often the "silver bullet" for medication-induced ED.
- Timing Matters: Sometimes taking your BP med at night instead of the morning can reduce the "peak" side effects during the day or evening.
- Lifestyle Synergy: Losing just 10 pounds can significantly lower blood pressure, potentially allowing you to reduce your dosage, which in turn reduces side effects.
Don't settle for a choice between your heart health and your intimate life. You can, and should, have both. Talk to your urologist or cardiologist openly. They’ve heard it all before, and they have the tools to fix it.