Seeing a thick, jelly-like blob on your pad or in the toilet can feel genuinely terrifying. You’re sitting there, staring down at something that looks like a piece of raw liver, and your brain immediately goes to the worst-case scenario. Is something tearing? Am I okay? Honestly, most of the time, those blood clots in the uterus that eventually make their way out are just a sign that your body is doing its job—albeit a bit too quickly for its own good.
It's messy. It's often painful. But it's also a very common physiological response.
When you’re menstruating, the lining of your uterus (the endometrium) sheds. To make this process smoother, your body releases anticoagulants—basically natural blood thinners—to keep the blood liquid so it can flow out easily. But when your flow is particularly heavy, the blood is moving so fast that those anticoagulants can't keep up. The blood pools in the vaginal vault or the uterus, and it clumps together. That’s how you end up with a clot.
The "Quarter Rule" and Why Size Matters
You've probably heard doctors mention the size of a quarter. It's the standard metric, though a bit arbitrary. If you're seeing clots smaller than a 25-cent coin, it’s usually just a "heavy day" thing. Nothing to freak out about. But when they start getting bigger than that—or if you're soaking through a maxi pad every single hour for several hours straight—that’s when we need to talk about Menorrhagia.
Menorrhagia isn't just "a bad period." It’s a clinical diagnosis for excessive menstrual bleeding. According to the Centers for Disease Control and Prevention (CDC), about 1 in 5 women deal with this, yet so many people just assume they’re "unlucky" once a month. They aren't just unlucky; they might have an underlying structural issue like fibroids or polyps that are physically getting in the way of the uterus contracting properly.
🔗 Read more: Exercises to Get Big Boobs: What Actually Works and the Anatomy Most People Ignore
Why Is My Uterus Making These?
Your uterus is a muscle. Its main job during a period is to contract and squeeze out the lining. If something is blocking that contraction, blood sits there. When blood sits, it clots. It’s a simple mechanical failure.
Uterine Fibroids are the most frequent culprits. These are non-cancerous growths in the muscular wall of the uterus. Think of them like little bumps in the road. They increase the surface area of the uterine lining, which means there is more tissue to shed, and they can also interfere with the muscle's ability to clamp down on blood vessels.
Then there’s Adenomyosis. This one is often misdiagnosed as "just bad cramps." It happens when the lining of the uterus starts growing into the actual muscular wall of the uterus. It makes the uterine wall thick and boggy. A "boggy" uterus doesn't contract efficiently, leading to—you guessed it—more blood pooling and larger clots.
Hormonal imbalances are the other side of the coin. If your estrogen and progesterone are playing tug-of-war, the lining can grow too thick (hyperplasia). When it finally sheds, it’s a landslide. This is super common during perimenopause or for those dealing with Polycystic Ovary Syndrome (PCOS).
💡 You might also like: Products With Red 40: What Most People Get Wrong
When the Clot Isn't Just a Period
We have to talk about the harder stuff. If you are pregnant—or think you might be—and you see blood clots in the uterus being expelled, you need to call a doctor immediately. It could be a miscarriage, or in some cases, an ectopic pregnancy. Sometimes, these clots are accompanied by a grayish tissue, which is a sign that it’s not just blood.
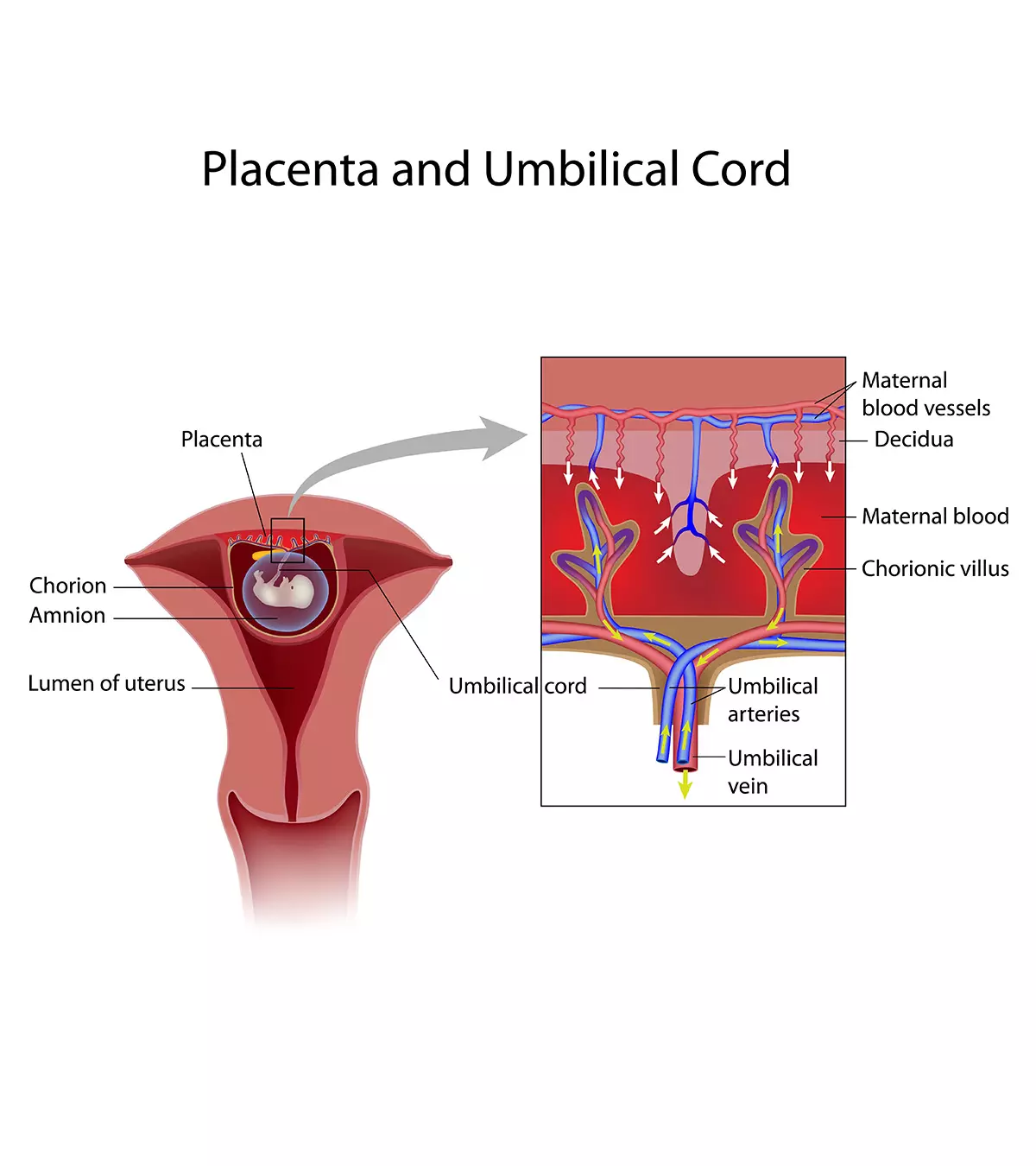
Postpartum is another "clot heavy" time. After giving birth, the site where the placenta was attached has to heal. You’ll experience lochia, which is the shedding of this tissue and blood. While some clotting is expected in those first few days, passing a "golf ball-sized" clot a week later is a red flag for retained products of conception or a late-term hemorrhage. Don't "wait and see" with that. Just go to the ER.
The Real Impact: Anemia and Fatigue
Let’s be real: losing this much blood is exhausting. If you’re passing large clots, you’re likely losing more iron than your body can replace. Chronic iron deficiency anemia makes you feel like you’re walking through underwater.
- You’re pale.
- Your heart races when you walk up a flight of stairs.
- You’re chewing ice (pica).
- You feel a level of tired that coffee can't fix.
Doctors like Dr. Jen Gunter, a noted OB-GYN and author of The Vagina Bible, often emphasize that women are frequently told their heavy bleeding is "normal" when it absolutely isn't. If your period is dictating your life—if you can’t leave the house because you’re afraid of "flooding" or passing a massive clot in public—that is a medical issue, not a lifestyle quirk.
📖 Related: Why Sometimes You Just Need a Hug: The Real Science of Physical Touch
Getting a Diagnosis That Actually Works
Don't let a GP just tell you to take some Ibuprofen and call it a day. If you're dealing with persistent blood clots in the uterus, you need a workup.
A pelvic ultrasound is usually the first step. It’s non-invasive and can spot fibroids or polyps easily. Sometimes, a doctor might want a Saline Infusion Sonohysterogram (SIS). They put a little bit of salt water into the uterus to expand it so the camera can see the shape of the cavity more clearly. It sounds uncomfortable, and it kind of is, but it’s the "gold standard" for finding out why the plumbing is backed up.
Blood tests are also non-negotiable. You need a CBC (Complete Blood Count) to check for anemia and a Ferritin test to see your iron stores. Standard iron tests can sometimes look "normal" even when your actual stores are depleted.
Treatment Options Beyond "The Pill"
For years, the default answer was "get on birth control." And while hormonal contraceptives can thin the uterine lining and reduce clots, they aren't the only way.
- Tranexamic Acid (Lysteda): This isn't a hormone. It’s a medication you take only during your period that helps your blood clot more effectively at the site, reducing the overall volume of blood you lose.
- IUDs (Mirena/Liletta): These release a tiny amount of progestin directly into the uterus. Many people stop having periods—and clots—entirely.
- Uterine Artery Embolization: If fibroids are the cause, a radiologist can essentially "starve" the fibroids by cutting off their blood supply.
- Myomectomy or Hysterectomy: If you're done having kids or the pain is too much, surgical removal of the fibroids or the uterus itself is a permanent fix.
Actionable Steps for This Month
If you are currently dealing with heavy clots, there are things you can do right now to manage the situation.
- Track the size. Honestly, take a picture if you have to. It feels gross, but showing your doctor the scale of the clots is way more effective than just saying "they’re big."
- Hydrate with electrolytes. You aren't just losing blood; you’re losing fluid and salts. Plain water isn't enough when you're hemorrhaging.
- NSAIDs are your friend. Ibuprofen or Naproxen doesn't just help with pain; it actually reduces the production of prostaglandins, which can technically lower your total blood loss by about 25-30%.
- Iron-rich foods + Vitamin C. If you're bleeding heavily, eat steak, spinach, or lentils, and pair them with orange juice to help absorption.
- Advocate for yourself. If your doctor dismisses your concerns, find a new one. Heavy clotting that interferes with your quality of life is a valid medical concern that deserves an investigation into the structural or hormonal root cause.
The bottom line is that while a few small clots are a normal part of the body's self-cleaning mechanism, large, frequent clots are a distress signal. Listen to it. Your uterus shouldn't be making you feel like a prisoner in your own home once a month.