It sounds like a movie plot, but it’s real. People are getting worried about H5N1 again. You’ve probably seen the headlines. They’re scary. But if you actually look at the data on bird flu human deaths, the reality is a lot more nuanced than a thirty-second news clip suggests. It’s not a simple "yes or no" situation regarding a pandemic. It’s a "maybe, and here is exactly why" situation.
Bird flu has been around for decades. We first saw H5N1 jump to humans in Hong Kong back in 1997. Since then, the world has been on edge. Why? Because when it does hit humans, it’s often brutal. We are talking about a virus that, historically, has a case fatality rate hovering around 50%. That is a massive number. To put it in perspective, COVID-19 was roughly 1% or less depending on the wave.
But there’s a catch.
Most of those historical bird flu human deaths happened in very specific circumstances. We’re talking direct, heavy contact with sick poultry. Think backyard farms or live bird markets. The virus hasn’t quite figured out how to hop from person to person easily. Yet.
The 2024-2025 Shift: Why Doctors Are Sweating
Something changed recently. H5N1 started showing up in cows. Cows! Nobody really saw that coming. In the United States, we’ve seen dozens of dairy herds across multiple states test positive. And then, the inevitable happened: farmworkers started testing positive too.
Richard Webby, a prominent virologist at St. Jude Children's Research Hospital, has been tracking this closely. He’s noted that while the current strain in the U.S. seems "milder" in humans—mostly causing conjunctivitis (pink eye) or mild respiratory issues—the risk of the virus mutating is always there.
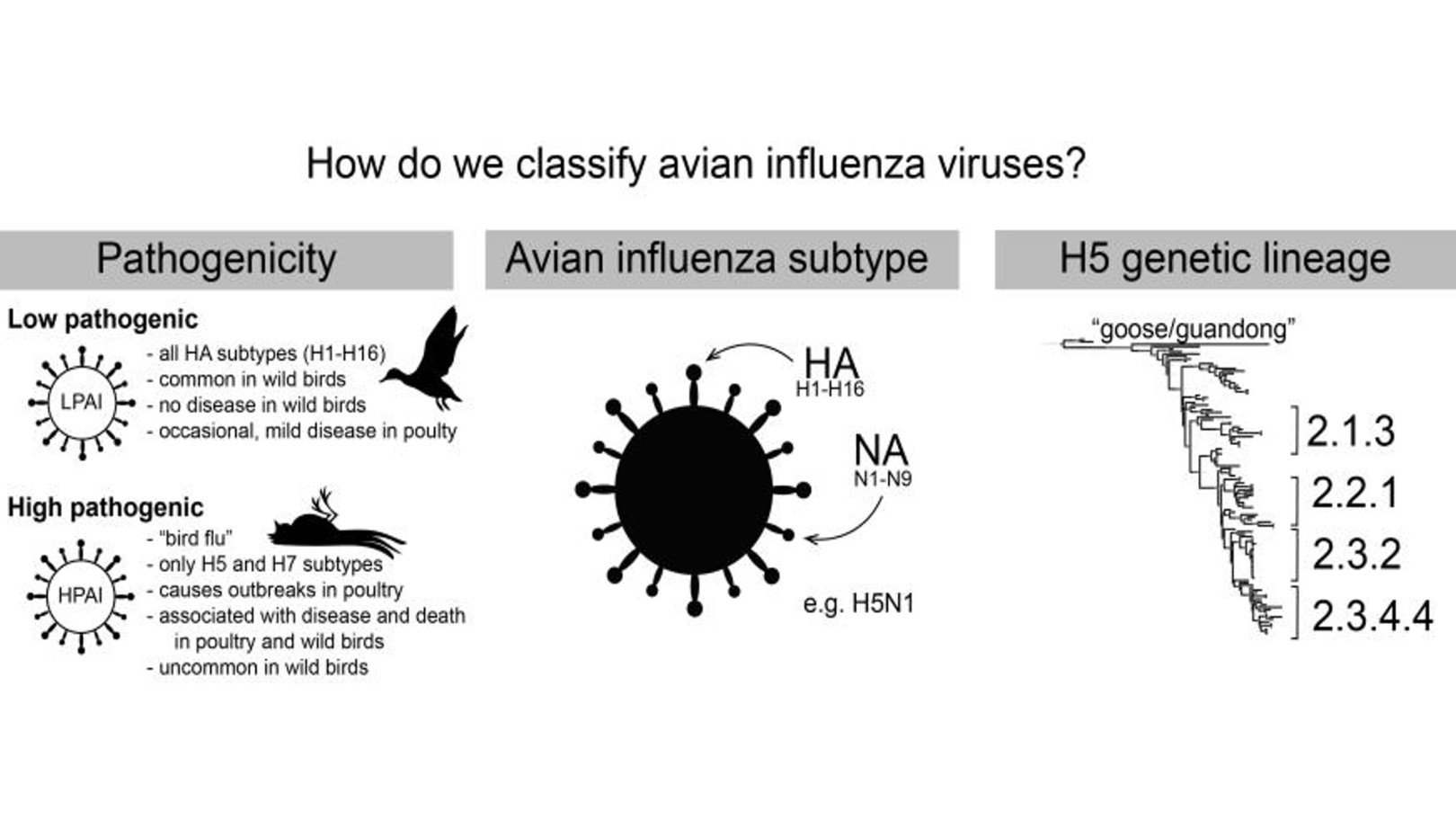
If you look at the recent timeline of bird flu human deaths, the numbers remain low, but the geographic spread is weird. We had a death in Mexico in 2024 involving the H5N2 strain. That was the first time that specific subtype was confirmed in a human globally. The patient had multiple underlying health conditions, which complicates the "cause of death" discussion, but the virus was there. It was a wake-up call that H5N1 isn't the only player on the field.
Breaking Down the Fatality Rates
You can't just look at one number. The World Health Organization (WHO) keeps a running tally. Since 2003, there have been nearly 900 laboratory-confirmed human cases of H5N1 reported from 23 countries. Out of those, more than 460 were fatal.
👉 See also: Why Your Best Kefir Fruit Smoothie Recipe Probably Needs More Fat
That looks terrifying on paper.
However, many experts believe the actual number of cases is much higher, meaning the death rate might be lower. If someone gets a mild cough and never goes to the hospital, they aren't a "confirmed case." We might only be seeing the absolute worst of the worst. This is a classic "ascertainment bias" in epidemiology.
What Actually Happens to the Body?
When H5N1 turns lethal, it isn't just a bad cold. It’s a cytokine storm. Your immune system basically panics. It floods the lungs with cells and fluid to fight the virus, but it ends up drowning the organs.
Most bird flu human deaths result from viral pneumonia and multi-organ failure. Unlike the seasonal flu, which usually sticks to the upper respiratory tract, H5N1 can get deep into the lung tissue. It binds to receptors that are more common deep in the human lower respiratory tract. This is actually a bit of a "silver lining"—because the virus is stuck deep down, it’s harder to cough out onto other people. If it mutates to bind to the upper throat and nose, that’s when we have a real problem.
The Missouri Mystery
Recently, a case in Missouri baffled everyone. A person tested positive for H5 without any known exposure to animals. No cows. No birds. No raw milk.
This is the kind of stuff that keeps CDC officials up at night. If there's no animal link, how did they get it? Was it "silent" human-to-human transmission? Testing of close contacts didn't show a massive outbreak, which is good news. But it highlights the gaps in our surveillance. We are basically flying a plane while still building the radar.
Raw Milk and the "Darwin Award" Factor
We have to talk about the raw milk trend. It’s honestly frustrating for public health officials. High levels of H5N1 have been found in the raw milk of infected cows. While pasteurization—heating the milk—kills the virus effectively, drinking it straight from the vat is like playing Russian roulette with your lungs.
✨ Don't miss: Exercises to Get Big Boobs: What Actually Works and the Anatomy Most People Ignore
The FDA conducted studies showing that even when the virus is present in milk, the bits left over after pasteurization are "dead" and can't infect you. But people are still seeking out raw milk as a "health food." This creates a direct bridge for the virus to move from the barnyard into suburban kitchens.
How to Actually Protect Yourself
Forget the panic-buying of masks for a second. The risk to the average person who doesn't work on a farm is currently "low." That’s the official word from the CDC, and the data backs it up. You aren't going to catch this walking down the street in Chicago or London.
But you should be smart.
- Stop touching dead birds. If you see a dead crow or duck in your yard, don't pick it up. Call local animal control. This is the most common way people get exposed.
- Cook your eggs and poultry. The virus is heat-sensitive. A runny egg is usually fine because the risk in commercial poultry is heavily monitored, but if there's an active outbreak in your area, maybe go for over-easy instead of raw.
- Avoid raw dairy. Seriously. Just don't do it right now. It’s an unnecessary risk for a "benefit" that isn't even scientifically proven.
Is a Vaccine Ready?
Yes and no. The U.S. government has a "seed strain" ready to go. They’ve actually started the process of bottling millions of doses of H5N1 vaccine. But here’s the kicker: it’s based on the current strain. If the virus mutates significantly to start spreading between humans, the vaccine might need an update.
It’s a game of cat and mouse.
Also, we have antivirals like Tamiflu (oseltamivir). Most current strains of bird flu are still sensitive to it. That's a huge advantage we didn't have in 1918. If someone is exposed and starts treatment early, the chances of bird flu human deaths dropping significantly are very high.
Why We Should Worry (But Not Panic)
The main concern isn't what the virus is doing today. It’s what it could do tomorrow. Every time a human gets infected, the virus gets a "practice run" at human DNA. It’s trying to figure out how to unlock the door to our species.
🔗 Read more: Products With Red 40: What Most People Get Wrong
We see this in pigs too. Pigs are "mixing vessels" because they can be infected by both bird flu and human flu at the same time. If a pig gets both, the viruses can swap segments of DNA—a process called reassortment. This could create a "Frankenvirus" that has the lethality of bird flu and the transmissibility of the common cold.
The Economic Reality of Bird Flu
This isn't just a health issue; it's a food security issue. Millions of chickens and turkeys have been culled to stop the spread. This is why your egg prices have been weird lately. When we talk about bird flu human deaths, we also have to consider the secondary effects—the stress on farmers, the loss of livelihoods, and the potential for a protein shortage if it hits the beef industry harder.
In 2024, the USDA began discussing a massive vaccination campaign for poultry. Some countries, like France, have already started. The U.S. has been hesitant because it complicates international trade—it’s hard to tell the difference between a vaccinated bird and a sick one with standard tests.
What the Experts are Watching
Keep an eye on the "H" and "N" numbers. We mostly talk about H5N1, but H7N9 and H9N2 are also on the watchlist. In 2013, H7N9 caused a significant spike in human cases in China. It was particularly scary because it didn't kill the birds, so they were "silent spreaders."
The current H5N1 strain is "highly pathogenic" in birds, meaning it kills them quickly. This is actually helpful for us because we know exactly where the virus is. If the birds stay healthy but carry the virus, we’re in trouble.
Immediate Steps You Can Take
While the threat level is low for the general public, staying informed is your best defense against both the virus and the misinformation surrounding it.
- Check the CDC Dashboard: They provide weekly updates on H5N1 in both livestock and human cases. It’s the most accurate source for domestic data.
- Practice Basic Hygiene: Washing your hands after being outdoors or handling grocery-store poultry isn't just for show. It works.
- Support Surveillance: If you live in a rural area, support local initiatives for testing wildlife and livestock. The faster we catch it in animals, the less likely it is to reach humans.
- Monitor Respiratory Symptoms: if you have had direct contact with farm animals or wildlife and develop a fever or cough, mention that specific animal contact to your doctor immediately. Early intervention with antivirals is the most effective way to prevent a severe outcome.
The situation with bird flu is evolving. It’s not a static threat. By understanding the difference between a "spillover" event and a "pandemic" event, you can keep your anxiety in check while remaining prepared for whatever comes next.
For now, the focus is on containment and science. We have the tools. We just need the coordination to use them before the virus makes its next move.