You’ve probably been told your whole life that 120/80 is the gold standard. It’s the number we all aim for, the one etched into every medical brochure since the eighties. But honestly? The "best blood pressure numbers" for you might look a lot different than they do for your neighbor, your spouse, or even your younger self. The medical community is currently in the middle of a massive shift in how we look at these digits. It isn’t just about hitting a specific target anymore; it’s about understanding the nuances of your own cardiovascular system.
Biology is messy.
If you walk into a doctor's office after fighting for a parking spot, your numbers will spike. That’s "White Coat Hypertension," and it’s real. If your doctor bases your entire treatment plan on that one five-minute window, they might be chasing a ghost. We need to talk about what these numbers actually represent and why the obsession with a single "perfect" score can sometimes do more harm than good.
The 120/80 myth and the SPRINT study
For decades, the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC) kept the bar at 140/90. If you were under that, you were "fine." Then came 2015. The Systolic Blood Pressure Intervention Trial (SPRINT), funded by the National Institutes of Health, changed everything. They looked at over 9,000 adults and found that those who pushed their systolic number—that top one—down to 120 had a 25% lower risk of cardiovascular events compared to those aiming for 140.
But here’s the kicker.
👉 See also: Finding the Right Fit: What You Need to Know About Rancho Mesa Care Center
The SPRINT study used high-tech, automated office blood pressure (AOBP) measurements where the patient sat alone in a quiet room. That almost never happens in a real clinic. In the real world, a nurse is chatting with you, your arm might be in the wrong position, or you’re worried about your co-pay. This discrepancy means that a "real world" 130 might actually be a "clinical" 120. Context is everything.
What the numbers actually mean
The top number, systolic, measures the pressure in your arteries when your heart beats. It’s the "thump." The bottom number, diastolic, measures the pressure when your heart rests between beats. Think of it like a garden hose. If the pressure is too high for too long, the hose starts to fray. Eventually, it bursts or leaks.
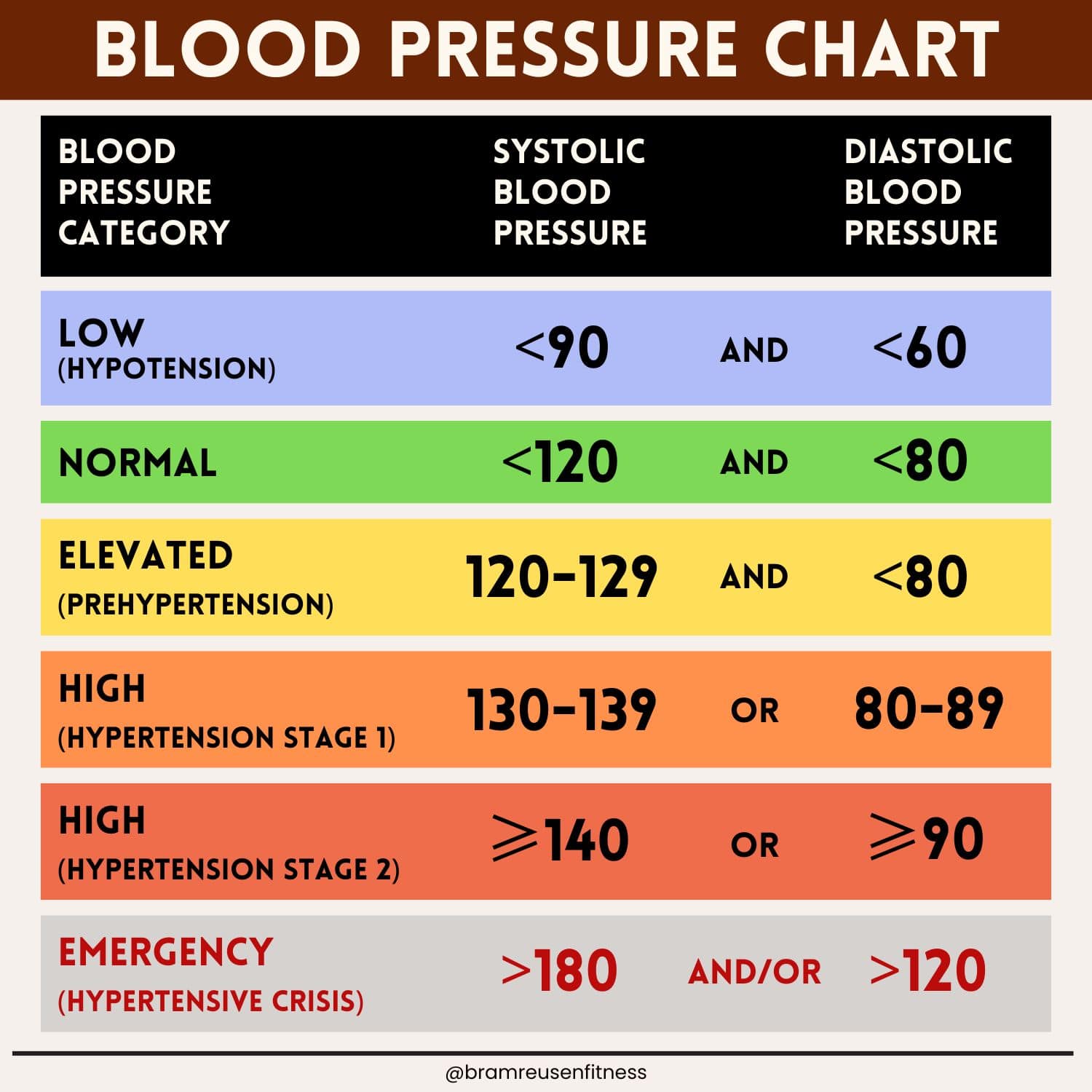
The American Heart Association (AHA) and the American College of Cardiology (ACC) updated their guidelines in 2017. They lowered the threshold for "Stage 1 Hypertension" to 130/80. Suddenly, millions of people who thought they were healthy were technically hypertensive. It caused a panic. But the goal wasn't to put everyone on meds. It was to wake people up to the fact that damage starts much earlier than we thought.
Best blood pressure numbers by age and stage
Your "best" number is a moving target. If you’re 25, 120/80 is great. If you’re 85? Pushing for 120/80 might actually be dangerous. Over-treating blood pressure in the elderly can lead to orthostatic hypotension—that dizzy feeling when you stand up. If an 80-year-old gets dizzy, they fall. If they fall, they break a hip. In that demographic, a "perfect" number might actually be 135/85 to ensure the brain gets enough blood flow.
Nuance matters.
- For most adults: Aiming for less than 130/80 is the standard recommendation for preventing long-term organ damage.
- For those with diabetes or kidney disease: The target is often even stricter because high pressure destroys the delicate filters in your kidneys.
- For the "frail" elderly: Doctors often tolerate higher numbers (up to 140 or 150 systolic) to prevent fainting and falls.
Dr. Sandra Taler from the Mayo Clinic has often pointed out that we have to balance the benefits of lower pressure against the side effects of the medications used to get there. Fatigue, leg swelling, and kidney stress are real trade-offs.
The "Morning Surge" and why one reading is useless
Your blood pressure isn't a static statue. It’s more like a stock market ticker. It’s lowest when you’re sleeping and starts to climb before you even wake up. This is the "morning surge," and it's when most strokes and heart attacks happen. If you only check your pressure at 2:00 PM after lunch, you’re missing the most dangerous part of your day.
You've got to track it at home.
The best way to find your true best blood pressure numbers is through Ambulatory Blood Pressure Monitoring (ABPM) or at least consistent home monitoring. Buy a validated cuff—check ValidateBP.org to see if yours is actually accurate. Many of the cheap ones from big-box stores are essentially random number generators.
Sit. Be quiet. Don't cross your legs. Don't use your phone.
Take two readings in the morning and two at night for a week. Average them out. That average is your real number. If your average is 128/78, but you hit 145/90 at the doctor's office, you have White Coat Hypertension. You probably don't need medication; you just need to breathe. Conversely, some people have "Masked Hypertension," where they look fine at the doctor but their pressure spikes at home due to work stress. That’s actually more dangerous because it goes untreated.
Salt, potassium, and the "Hidden" pressure levers
We talk about salt constantly. "Cut the sodium!" is the mantra. And yeah, for about half the population, salt is a major trigger. But for the other half, it doesn't do much. What people ignore is potassium.
Potassium is the "anti-salt." It helps your kidneys flush out sodium and eases the tension in your blood vessel walls. If you’re tracking your best blood pressure numbers, you should be tracking your potassium intake too. Bananas are the cliche, but avocados, spinach, and potatoes actually have more.
The DASH diet (Dietary Approaches to Stop Hypertension) isn't just a fad. It’s one of the most rigorously studied eating plans in medical history. It can drop your systolic pressure by 8 to 14 points. That’s as effective as some medications.
🔗 Read more: Collagen Peptides Explained: What Actually Happens When You Take Them
The silent killers of your "Best" numbers
Sleep apnea is the big one. If you snore and wake up tired, your blood pressure is likely screaming at night. Every time you stop breathing, your body enters a "fight or flight" mode, dumping adrenaline into your system. This spikes your pressure. If you don't fix the apnea, the blood pressure meds won't work well.
Alcohol is another "sneaky" culprit. You might think a glass of red wine is heart-healthy, but more than one or two drinks actually raises blood pressure. It’s a dose-dependent relationship. The more you drink, the higher the baseline goes.
And then there's stress. Not just "I had a bad day" stress, but chronic, systemic stress. The kind that keeps your cortisol high. You can eat all the kale in the world, but if your nervous system is constantly red-lined, your blood pressure will follow suit.
Actionable steps for your cardiovascular health
Stop obsessing over a single reading and start looking at the trend. Your body is an ecosystem, not a machine with fixed settings. To find and maintain your best blood pressure numbers, you need a strategy that goes beyond the pill bottle.
📖 Related: How Can I Get Drunk Faster: The Science of Blood Alcohol Concentration
- Validate your equipment. If your home monitor isn't validated, your data is garbage. Take your home cuff to your next doctor's appointment and calibrate it against theirs.
- The 5-minute rule. Never take your pressure the second you sit down. Sit still for five minutes. No talking. No TV. This is the only way to get a "resting" heart rate and pressure.
- The Potassium/Sodium Ratio. Instead of just cutting salt, try to double your potassium. This "ratio" approach is often more sustainable and effective for vascular health.
- Check your neck. If you have high blood pressure that won't budge despite meds, get a sleep study. Treating apnea is often the "magic bullet" for stubborn hypertension.
- Watch the "bottom" number in younger years. In people under 50, a high diastolic (bottom) number is often a better predictor of future heart issues. As we age, the arteries stiffen, and the systolic (top) number becomes the primary concern.
- Don't ignore 130. If you're consistently hitting 130-135 systolic, don't wait for it to hit 140. This is the "yellow light" phase. Small changes here—like a 15-minute daily walk—can prevent the need for lifelong medication later.
Blood pressure is the leading cause of preventable death globally, mostly because it doesn't "feel" like anything until it's too late. You won't feel your 150/95. You’ll feel the stroke it causes ten years from now. Get your data, understand your personal baseline, and work with a provider who looks at you as a human, not just a set of digits on a screen.