You’re sitting in a cold doctor's office, and they’ve just told you that you have a nasty sinus infection or maybe a strep throat that won't quit. Then comes the inevitable question: "Any allergies?" You say you're allergic to penicillin and cephalosporins. Suddenly, the vibe shifts. The doctor looks at their screen, starts scrolling, and you realize your options for getting better just got a whole lot more complicated.
It's a common story.
Roughly 10% of the U.S. population reports a penicillin allergy. However, here is the kicker: about 90% of those people aren't actually allergic when they get tested. We’ve been carrying around these labels since we were toddlers because our moms saw a rash once and, naturally, freaked out. But when you add cephalosporins into the mix, things get dicey because these two classes of drugs are basically cousins.
The family tree of Beta-Lactams
To understand why being allergic to penicillin and cephalosporins is such a headache, you have to look at their "bones." Both belong to a group called beta-lactam antibiotics. They both have a specific chemical ring—the beta-lactam ring—that acts like a key to unlock and destroy bacterial cell walls.
Because they look so much alike, your immune system can get confused.
In the old days, doctors thought if you were allergic to penicillin, you had a massive chance of reacting to cephalosporins too. We’re talking 10% or higher. Modern research, like the stuff published in The Journal of Allergy and Clinical Immunology: In Practice, shows that the "cross-reactivity" is actually much lower—closer to 1% or 2% for most people.
Why the change?
📖 Related: Why That Reddit Blackhead on Nose That Won’t Pop Might Not Actually Be a Blackhead
Back in the 60s and 70s, cephalosporins were often contaminated with traces of penicillin during the manufacturing process. It wasn't always the drug itself; it was the "dirt" in the recipe. Today, manufacturing is pristine. The real danger usually lies in the "side chains" of the chemical structure. If a specific penicillin (like Amoxicillin) has a side chain that looks identical to a specific cephalosporin (like Cephalexin), your body might attack both. If they don't match? You’re probably fine.
The "False" Allergy Trap
Most people who think they are allergic to penicillin and cephalosporins are living a lie. That sounds harsh, but it’s medically true.
Think back. Were you three years old? Did you have a pink, itchy rash while taking Amoxicillin for an ear infection? Many viral infections—like Roseola or even Mono—cause rashes that look exactly like an allergic reaction. The doctor plays it safe, puts "PENICILLIN ALLERGY" in your chart in big red letters, and you spend the next thirty years avoiding the best, cheapest, and most effective antibiotics on the planet.
Also, allergies fade.
Even if you were truly allergic as a kid, about 80% of people lose that sensitivity after a decade. Your immune system basically forgets to be mad at the drug. But that "allergy" label stays in your electronic health record like a permanent stain, following you from clinic to clinic.
What a real reaction looks like
If you're genuinely allergic, it’s not just a few stray hives that disappear with Benadryl. We are talking about IgE-mediated responses.
👉 See also: Egg Supplement Facts: Why Powdered Yolks Are Actually Taking Over
- Anaphylaxis: This is the big one. Throat closing, drop in blood pressure, feeling like you're dying.
- Angioedema: Serious swelling, usually in the face, lips, or tongue.
- Wheezing: Your lungs tightening up within minutes of taking the pill.
- Late-stage reactions: These are rarer but scarier, like Stevens-Johnson Syndrome (SJS), where your skin literally starts to peel off. If you’ve had SJS, you stay away from the trigger drug forever. No exceptions.
Why this label is actually dangerous for you
You might think, "Who cares? I'll just take something else."
Honestly, that’s a risky mindset. When you can’t take penicillin or cephalosporins, doctors have to move to "broad-spectrum" or "big gun" antibiotics like vancomycin, clindamycin, or fluoroquinolones (like Cipro). These drugs are often harder on your body. They kill off all the good bacteria in your gut, which opens the door for C. diff, a nightmare infection that causes relentless diarrhea and can land you in the hospital.
Also, broad-spectrum drugs contribute to antibiotic resistance. We are basically training bacteria to be "superbugs" because we can't use the simple, targeted stuff. Using the wrong antibiotic can lead to longer hospital stays and higher medical bills. It is a domino effect of bad news.
Navigating the Cephalosporin "Generations"
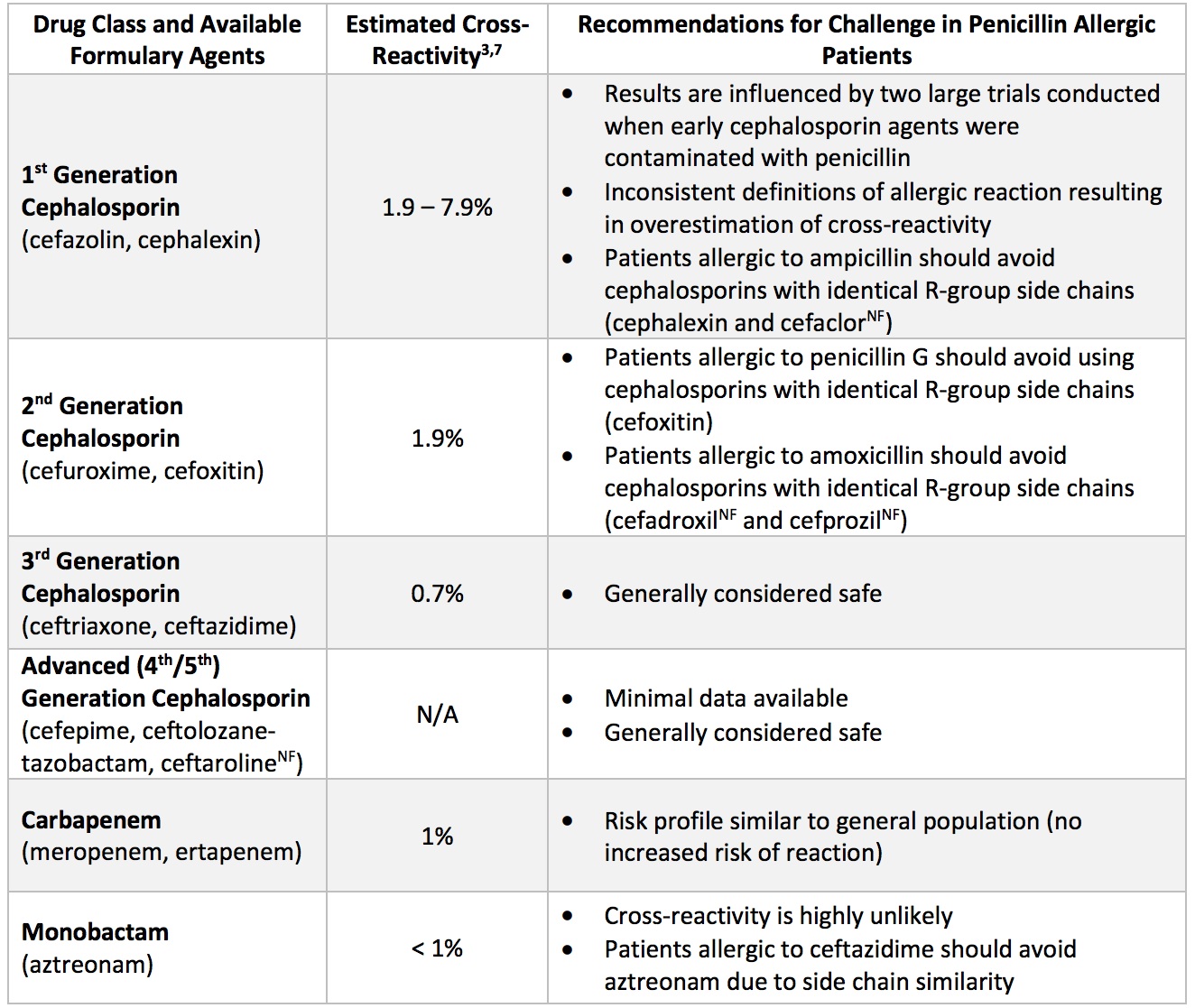
Cephalosporins aren't just one drug. They are a massive family divided into "generations."
- First Generation (e.g., Cephalexin/Keflex): These are the closest relatives to penicillin. If you have a confirmed, severe penicillin allergy, these are the ones most likely to cause a cross-reaction.
- Third and Fourth Generations (e.g., Ceftriaxone/Rocephin or Cefepime): These are the distant cousins. The chemical structures have diverged so much that many people with a penicillin allergy can tolerate these perfectly fine.
Dr. Kimberly Blumenthal from Massachusetts General Hospital has done extensive work on this. Her research basically suggests that we are over-avoiding these drugs. If a patient needs a third-generation cephalosporin for a lung infection, the risk of a life-threatening reaction is statistically tiny, even with a penicillin allergy on file.
What you should do next
Don't just sit there with a potentially fake allergy on your record. Take control of your chart.
✨ Don't miss: Is Tap Water Okay to Drink? The Messy Truth About Your Kitchen Faucet
Get a referral to an Allergist. This is the gold standard. They will do a skin prick test. It takes about an hour. They poke your skin with a tiny bit of the drug and wait to see if a "wheal" (a bump like a mosquito bite) appears. If that's negative, they might do an "oral challenge." They give you a small dose of the actual antibiotic and watch you for an hour.
If you pass the oral challenge, you are officially "de-labeled."
It is a liberating feeling. Suddenly, the pharmacy isn't a minefield anymore. You can take the $4 generic Amoxicillin instead of the $100 "alternative" that makes you nauseous.
Update your pharmacy and every portal. If you get cleared, don't assume the hospital knows. You have to manually tell your primary care doctor, your dentist, and your pharmacist to delete that allergy. You don't want a "ghost" allergy popping up in an emergency room five years from now when you're unconscious and need life-saving meds.
Ask about "Graded Challenges." If your doctor is nervous but you really need a cephalosporin, ask about a graded challenge. They give you 1/10th of the dose, wait, then give the rest. It’s a way to dip your toe in the water under medical supervision.
Actionable steps for the "Allergic" patient
- Audit your history: Ask your parents or look at old records. What actually happened? If it was just an upset stomach or a yeast infection, that’s a side effect, not an allergy.
- See an expert: Schedule a penicillin skin test. It is the only way to be 100% sure.
- Know the names: Learn to recognize the "Cef-" prefix (Cefdinir, Ceftriaxone, Cefuroxime). If you know you react to these, keep a list of the specific ones, as you might be fine with others in the same family.
- Carry a card: If your allergy is real and severe (anaphylaxis), wear a medical alert bracelet. In a car accident, the first thing an EMT might reach for is a beta-lactam antibiotic for trauma-related infections.
Being allergic to penicillin and cephalosporins isn't a life sentence of bad medicine, but it does require you to be an active participant in your own healthcare. Stop guessing and get the data. Your gut microbiome—and your wallet—will thank you.