You’re probably familiar with that heavy, "rock in the stomach" feeling after a massive Thanksgiving dinner. That’s normal. What isn’t normal is feeling like your digestive system is a battlefield every single day. Bad gut health symptoms aren't just about whether or not you need to run to the bathroom after a cup of coffee. It’s deeper. It’s about how your skin looks, how your brain processes a difficult task at 3:00 PM, and why you’re suddenly catching every cold that wanders through the office.
The gut is basically the body’s second brain.
Honestly, it might even be the first brain when you consider that the enteric nervous system contains over 100 million nerve cells. When things go south in the microbiome—the trillions of bacteria, fungi, and viruses living in your intestines—the fallout is messy. It isn't always a stomach ache. Sometimes, it’s just a weird rash on your elbow or a level of fatigue that three espressos can't fix.
The Bathroom Habit Trap
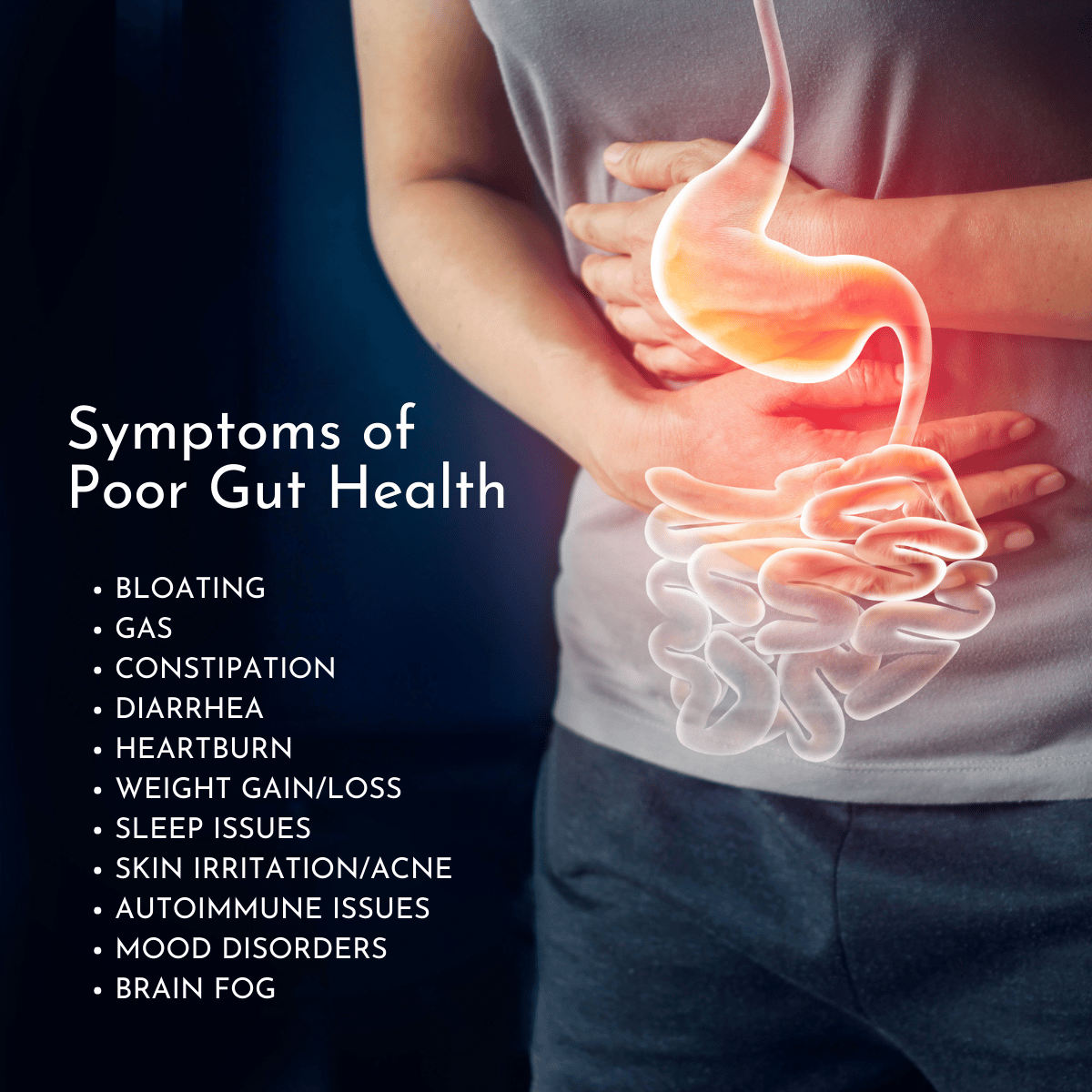
Most people think "bad gut health symptoms" starts and ends with bloating. While bloating is a massive red flag, especially if it happens regardless of what you eat, the real data is in the frequency. Consistency matters.
If you’re swinging wildly between "I can't go" and "I can't stop going," your microbiome is screaming for help. This is often a sign of dysbiosis, which is just a fancy way of saying your bad bacteria have staged a coup against the good ones. Dr. Will Bulsiewicz, a prominent gastroenterologist and author of Fiber Fueled, often points out that our modern diet—high in processed "ultra-palatable" foods—acts like a weed killer for our internal garden. When the garden dies, the soil (your gut lining) gets leaky.
Small Intestinal Bacterial Overgrowth (SIBO) is another culprit that gets misdiagnosed as generic IBS. With SIBO, the bacteria that should be in your large intestine migrate up into the small intestine. They start fermenting food way too early. The result? Gas that feels like a balloon is inflating under your ribcage. It's painful. It's embarrassing. And it’s a classic symptom that something is fundamentally broken in your digestive rhythm.
Beyond the Belly: The Skin and Mood Connection
Your face is a map of your gut.
💡 You might also like: How Much Should a 5 7 Man Weigh? The Honest Truth About BMI and Body Composition
Ever notice a breakout right after a weekend of eating nothing but pizza and beer? That’s the gut-skin axis in action. Research published in journals like Frontiers in Psychology has shown that systemic inflammation, triggered by a compromised gut barrier, travels. It doesn't stay in the colon. It hits the bloodstream. Once those inflammatory markers are circulating, they often manifest as acne, rosacea, or even psoriasis flare-ups.
Then there’s the mental fog.
If you feel like you’re walking through a cloud, check your digestion. Roughly 95% of your body's serotonin is produced in the gut. If the environment is toxic, your neurotransmitter production hits a wall. You aren't just "tired"; you’re chemically incapable of feeling sharp. This isn't some "woo-woo" wellness theory; it’s biology. The vagus nerve acts as a high-speed data cable between your gut and your brain. When the gut is inflamed, it sends "danger" signals to the brain, which can manifest as anxiety or low-level depression.
Why "Healthy" Food Sometimes Makes it Worse
This is the part that trips everyone up. You decide to "get healthy," so you start eating massive salads and drinking green smoothies. Suddenly, your bad gut health symptoms get worse. You’re more bloated than ever.
Why?
Because if your gut wall is already damaged, or if you have a lack of microbial diversity, you can't handle the fiber. It’s like trying to run a marathon on a broken leg. High-FODMAP foods (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) like garlic, onions, and broccoli are "healthy," but they are also fuel for fermentation. If you have an overgrowth of the wrong bacteria, these foods just feed the fire.
📖 Related: How do you play with your boobs? A Guide to Self-Touch and Sensitivity
Sugar Cravings are a Bio-Hack
Have you ever felt like you physically couldn't resist a cookie? It might not be a lack of willpower. Certain types of yeast, like Candida albicans, thrive on sugar. When they become dominant in your gut, they can actually influence your cravings by releasing signaling molecules that change your taste preferences and mood. They are literally hacking your brain to get fed.
- Weight Fluctuations: Unexpected weight gain or loss, despite no change in diet, can signal malabsorption or insulin resistance triggered by gut bacteria.
- Autoimmune Flare-ups: A "leaky gut" allows undigested food particles into the blood, causing the immune system to go into overdrive and attack its own tissues.
- Constant Fatigue: If your gut can't absorb B12 or magnesium, you will be exhausted no matter how much you sleep.
- Sleep Issues: Since the gut regulates melatonin precursors, a bad microbiome often leads to insomnia or fragmented sleep.
The Role of Stress and Antibiotics
We have to talk about the "scorched earth" policy of antibiotics. While they are lifesaving, they are the nuclear bombs of the microbial world. One course can disrupt your gut flora for months, or even years, if you don't actively work to rebuild it. Most people finish their pills, feel better from their sinus infection, and then wonder why they have heartburn three weeks later.
Stress is the other silent killer. When you’re in "fight or flight" mode, your body shunts blood away from the digestive system. It thinks you’re being chased by a predator; it doesn't care about digesting your kale salad. Chronic stress keeps the gut in a state of low-level ischemia (restricted blood flow), which weakens the protective mucus lining. This makes you vulnerable to everything from ulcers to H. pylori infections.
Real-World Steps to Fix the Damage
Stop guessing. If you've been living with these symptoms for more than a month, you need data.
First, consider a temporary elimination diet. The Low-FODMAP diet is the gold standard for identifying triggers, but it’s not meant to be permanent. It’s a diagnostic tool. You cut out the common offenders for 2-4 weeks, then slowly reintroduce them one by one to see which one causes the flare-up.
Second, focus on diversity. The American Gut Project found that people who eat more than 30 different types of plants per week have significantly more diverse microbiomes than those who eat fewer than ten. A "plant" isn't just lettuce. It’s nuts, seeds, spices, grains, and fruits.
👉 See also: How Do You Know You Have High Cortisol? The Signs Your Body Is Actually Sending You
Third, get dirty. We live in a world that is too sterile. Spending time outdoors, gardening, or even just having a pet can introduce beneficial environmental microbes back into your system.
Fourth, prioritize fermented foods over expensive supplements. While a high-quality probiotic can help, foods like unpasteurized sauerkraut, kimchi, kefir, and miso provide a complex matrix of bacteria that a pill often can't match. Start small—literally a tablespoon a day—to avoid overwhelming your system.
Fifth, watch the timing. Give your gut a break. Migrating Motor Complex (MMC) is the "housekeeping" wave that sweeps through your intestines to clear out debris. It only happens when you aren't eating. Constant snacking prevents this process. Try to leave at least 3-4 hours between meals to let the MMC do its job.
Moving Forward With Intention
Understanding bad gut health symptoms requires a shift in perspective. You aren't just a body that processes food; you are a walking ecosystem. When that ecosystem is balanced, everything feels easier. When it’s not, life feels like an uphill climb.
Start by tracking your "Bristol Stool Chart" type and your energy levels in a simple journal for seven days. Look for patterns. Did that sourdough bread cause the brain fog, or was it the late-night stress scrolling? Once you identify the triggers, you can stop managing symptoms and start fixing the root cause. Your gut is resilient, but it needs the right environment to heal. Give it the fiber, the rest, and the diverse nutrients it needs, and the symptoms will usually take care of themselves.