Your heart is a muscle, sure, but it's also a sort of biological metronome that refuses to stay in time. Sit down, take a breath, and press two fingers against your wrist. That steady thump-thump is your average resting heart rate in action. Most of us grew up hearing that 72 beats per minute is the gold standard. It's the number in the textbooks. But honestly? That number is kind of a myth. Or at least, it's a very narrow slice of a much bigger, much weirder pie.
For the majority of adults, a "normal" range is actually anywhere between 60 and 100 beats per minute (bpm). That is a massive gap. It's the difference between a leisurely stroll and a brisk walk, yet both are technically considered "fine" by the American Heart Association. If you're sitting at 62 and your best friend is at 88, you aren't necessarily "healthier" in a vacuum. Context matters more than the raw digit on your Apple Watch or Fitbit.
The Science of the Squeeze
When we talk about the average resting heart rate, we are looking at the lowest amount of blood your body needs when you aren't doing anything. Think of it like a car idling in the driveway. If the engine is efficient, it doesn't need to rev high to stay running. If the engine is struggling or if it's a high-performance racing model, that idle speed changes.
Your autonomic nervous system runs the show. Specifically, the sympathetic nervous system (the "fight or flight" side) and the parasympathetic nervous system (the "rest and digest" side) are constantly playing tug-of-war. According to Harvard Health Publishing, your heart rate is a direct reflection of this internal balance. If you're stressed, the sympathetic system wins and your rate climbs. If you’re deep in a meditation session, the parasympathetic system takes over, and things slow down.
Why Athletes Break the Rules
You might have heard stories about elite marathoners or Tour de France cyclists having resting heart rates in the 30s or 40s. This is often called "Athletic Bradycardia." To a doctor treating a sedentary 80-year-old, a heart rate of 38 bpm might look like a medical emergency. But for someone like Miguel Induráin—a legendary cyclist who reportedly had a resting heart rate of 28 bpm—it's just a sign of an incredibly powerful pump.
When you exercise consistently, your heart muscle gets physically larger and stronger (left ventricular hypertrophy). It can push out more blood with every single contraction. This is known as stroke volume. Because it's moving so much blood per squeeze, it doesn't have to squeeze as often. It’s efficient. It's basically a heavy-duty diesel engine versus a buzzing weed-whacker.
💡 You might also like: How many calories is water? The real answer behind that zero on the label
The Hidden Variables You Probably Ignore
Most people check their heart rate once, see a number they don't like, and freak out. That's a mistake. Your average resting heart rate isn't a static statue; it's a moving target.
Dehydration is a huge factor that people overlook. When you're low on fluids, your blood volume actually drops. To keep your blood pressure stable and move oxygen around, your heart has to beat faster to make up for the lack of "stuff" to pump. If you’ve had a few drinks the night before, your heart rate will likely be elevated the entire next day. Alcohol is a double whammy: it dehydrates you and irritates the nervous system.
Temperature plays a role too. If it’s 95 degrees out and humid, your heart has to work harder to shunt blood to the surface of your skin to cool you down. You might see a jump of 10 bpm just from standing in the sun. Then there's the "White Coat Effect." Research published in the Journal of the American College of Cardiology suggests that many patients show significantly higher heart rates in a clinical setting just because they’re nervous about being at the doctor.
Age, Gender, and the Genetic Lottery
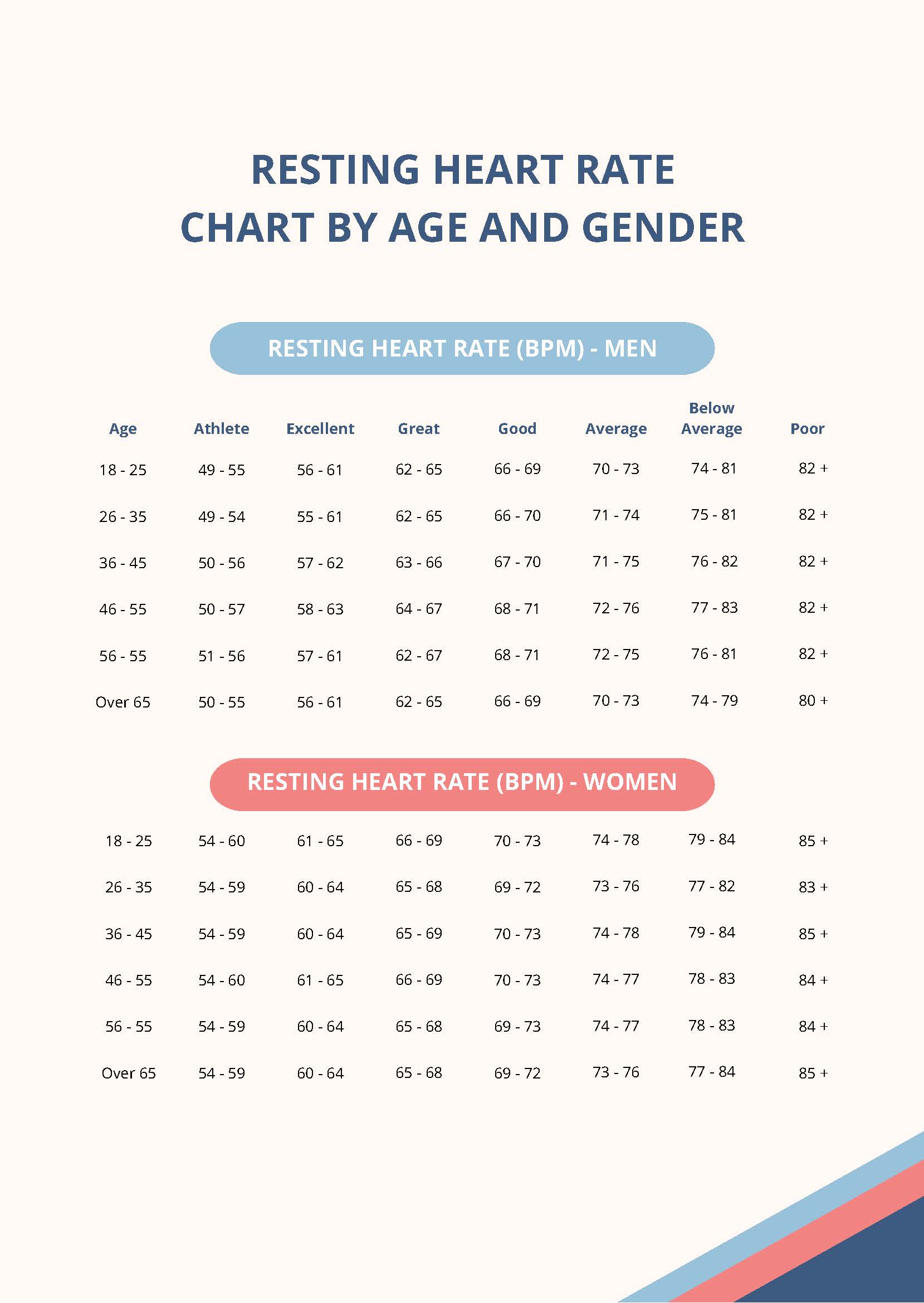
As we get older, the heart’s maximum capacity tends to drop, but the resting rate doesn't necessarily follow a straight line. Interestingly, women tend to have slightly higher average resting heart rates than men—usually by about 2 to 7 beats per minute. This isn't a fitness "fail." It's mostly down to heart size; women generally have smaller hearts, which need to beat a bit more frequently to move the same relative amount of blood.
The Danger Zones: When to Actually Worry
While the 60–100 range is "normal," there are outliers that demand attention. Tachycardia is the medical term for a resting heart rate over 100. If you are sitting on the couch and your heart is hammering away at 110 bpm, something is up. It could be caffeine, it could be thyroid issues, or it could be an underlying arrhythmia like Atrial Fibrillation (AFib).
On the flip side, Bradycardia (below 60 bpm) is only a problem if it's accompanied by symptoms. If your rate is 52 but you feel dizzy, short of breath, or like you’re about to faint, that’s a red flag. If it's 52 and you feel like a million bucks, you might just be in great cardiovascular shape.
The Mortality Connection
Is a lower heart rate always better? Generally, yes. A massive study published in the journal Heart tracked about 3,000 men for 16 years. They found that a higher resting heart rate was linked to a higher risk of mortality, even in healthy individuals. Specifically, those with a resting rate between 81 and 90 had a doubled risk of death compared to those with lower rates. Those over 90 tripled it.
This doesn't mean you're doomed if your heart beats fast. It just means that a high average resting heart rate is often a "proxy" for other issues like high inflammation, low physical activity, or chronic stress. It's a smoke detector, not the fire itself.
How to Get an Accurate Reading
Don't trust a single snapshot. To find your true average resting heart rate, you need to be consistent.
- The Morning Method: Check your pulse the second you wake up, before you even get out of bed. No coffee. No scrolling through stressful emails. Just you and the mattress.
- The Three-Day Average: Do this for three mornings in a row and take the average. This smooths out any weirdness from a bad night's sleep or a late-night pizza.
- The Finger Check: While wearables are great, they can be "noisy." For a true reading, use your index and middle finger on your radial artery (thumb side of the wrist). Count the beats for 30 seconds and multiply by two. Don't use your thumb—it has its own pulse and will confuse you.
Shifting the Needle
If you find your numbers are creeping into the 80s or 90s and you want to bring them down, you aren't stuck there. The heart is remarkably plastic.
- Zone 2 Cardio: This is the magic "sweet spot." It’s exercise where you can still hold a conversation but you're definitely working. Think of a light jog or a power walk. Doing this for 150 minutes a week strengthens the heart's walls and improves efficiency more than short, violent bursts of sprinting ever will.
- Magnesium and Potassium: These electrolytes are essential for the electrical signaling of the heart. If you're deficient, your heart might "stutter" or beat faster.
- Sleep Hygiene: Poor sleep triggers cortisol. Cortisol keeps your heart rate elevated. Even one night of 4 hours of sleep can spike your resting rate the following day by 5–10 bpm.
- Vagal Tone: Deep belly breathing—specifically making your exhales longer than your inhales—stimulates the Vagus nerve. This sends a direct signal to the heart to "chill out."
It's easy to get obsessed with the data. We live in an era of "The Quantified Self," where every heartbeat is logged in a cloud. But remember that your average resting heart rate is a trend, not a verdict. It’s a conversation your body is having with you. If the conversation is getting a bit too loud or fast, it’s usually an invitation to change a few habits rather than a reason to panic.
Actionable Next Steps
Start by establishing your baseline. Tomorrow morning, before you touch your phone, find your pulse. Do this for a full week. Record the numbers in a simple note on your phone. If you notice your average is consistently above 85 bpm, look at your hydration and sleep first. If those are dialed in and the number stays high, it's worth a chat with a doctor to rule out things like anemia or thyroid imbalances. On the other hand, if you’re seeing a steady decline as you start a new walking routine, take it as a win. Your heart is getting stronger, one beat at a time.