Ever find yourself staring at your Apple Watch or Garmin in the middle of the night, wondering why your pulse is thumping at 58 beats per minute while your partner’s is hitting 72? It’s a weirdly personal metric. We check it constantly. Yet, most of us actually have no clue what a "good" number looks like for our specific body. We’ve been told that 60 to 100 is the "normal" range, but honestly, that’s a massive gap. It’s like saying a normal height for a human is between four feet and seven feet. Technically true? Yeah. Helpful for you specifically? Not really.
Your average heart rate resting is basically the baseline of your internal engine. It's how many times your heart beats when you’re absolutely chill—usually first thing in the morning before the coffee kicks in or the kids start screaming. If that number is creeping up or dipping too low, your body is trying to tell you something about your stress, your fitness, or even an underlying infection you don't feel yet.
The 60 to 100 Range is Kinda Dated
The American Heart Association still sticks to that 60–100 beats per minute (bpm) standard for adults. It’s the safe bet. But if you talk to cardiologists at places like the Cleveland Clinic, they’ll tell you that most healthy adults should probably be sitting somewhere between 50 and 70 bpm.
Why the discrepancy?
Well, the "100" upper limit includes a lot of people who might be sedentary or dealing with chronic stress. If your resting heart rate is consistently hovering at 95, you’re technically "normal," but your heart is working a lot harder than someone at 65. Think of it like a car idling. A car idling at 3,000 RPMs is going to wear out its engine way faster than one idling at 900.
There’s a pretty famous study published in the journal Heart that tracked middle-aged men for years. They found that those with a resting heart rate higher than 90 bpm had triple the risk of dying compared to those in the lowest categories. That’s a heavy stat. It suggests that while 90 is "normal" by the old books, it’s not exactly "optimal" for longevity.
Does Fitness Always Lower It?
Mostly, yes. When you do a lot of cardio, your heart muscle gets stronger. It becomes a more efficient pump. It can push out more blood with a single squeeze, so it doesn't have to beat as often. This is why elite marathoners like Eliud Kipchoge or pro cyclists often have resting heart rates in the 30s or low 40s.
But don't panic if you’re a gym rat and your heart rate is still 68. Genetics plays a massive role here. Some people just have smaller hearts or different electrical conduction systems. You can't purely "exercise" your way into a 40 bpm pulse if your biology isn't wired for it.
👉 See also: How do you play with your boobs? A Guide to Self-Touch and Sensitivity
What's Actually Messing With Your Number?
It isn't just about how many miles you ran yesterday. A million little things tug at your heartstrings—literally.
Dehydration is a huge one.
When you’re low on fluids, your blood volume drops. Your blood gets a little thicker, a little harder to move. To keep your blood pressure stable, your heart has to kick it into gear and beat faster. If you wake up and see your average heart rate resting is 5-10 beats higher than usual, grab a glass of water. You're probably just parched.
The "Alcohol Tax"
If you have two or three glasses of wine at dinner, your heart rate will likely stay elevated all night. Alcohol is a vasodilator initially, but the metabolic byproduct—acetaldehyde—and the subsequent stress on your nervous system keep your pulse racing while you sleep. Many people using Oura rings or Whoop straps notice their "recovery" score tanks because their resting heart rate jumped from 55 to 68 after a night out.
Stress and the Sympathetic Nervous System
We live in a state of "micro-stress." Emails. Traffic. The news. This keeps our "fight or flight" system (the sympathetic nervous system) on a low-grade simmer. This releases cortisol and adrenaline, which tells the heart to speed up. It’s not a malfunction; it’s your body preparing for a threat that never actually shows up.
Temperature Matters
Heat makes your heart work harder. If your bedroom is too hot, or if you’re dealing with a fever, your heart rate climbs. For every degree your internal temperature rises, your heart rate usually goes up by about 10 beats per minute.
When Should You Actually Worry?
Low heart rate, or bradycardia, isn't always a badge of honor for being fit. If your rate is 45 but you feel dizzy, fatigued, or like you’re going to faint, that’s a problem. It could mean your heart isn't pushing enough oxygenated blood to your brain.
On the flip side, tachycardia (a resting rate over 100) needs a look from a pro.
✨ Don't miss: How Do You Know You Have High Cortisol? The Signs Your Body Is Actually Sending You
If you notice a sudden, sustained jump in your average heart rate resting that stays there for more than a few days, it’s worth a call to the doctor. It could be thyroid issues—specifically hyperthyroidism—or even anemia. When you don't have enough red blood cells to carry oxygen, your heart tries to compensate by speeding up the delivery.
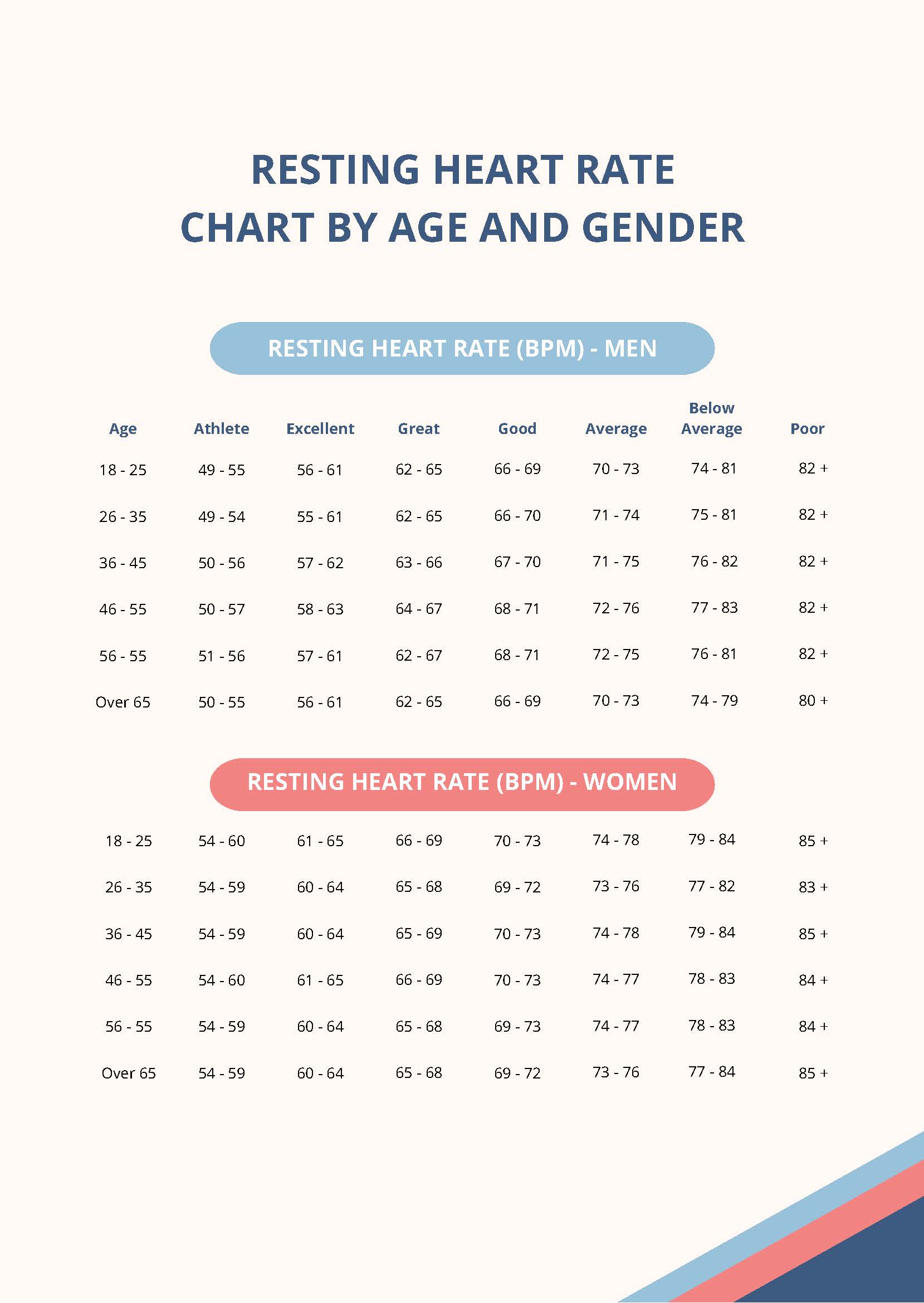
The Nuance of Age and Gender
It’s worth noting that women tend to have slightly higher resting heart rates than men. This is largely because women, on average, have smaller hearts that need to beat a bit more frequently to move the same amount of blood.
Age also changes things. Interestingly, resting heart rate doesn't necessarily "slow down" just because you get older, but your maximum heart rate definitely does. The gap between your rest and your max (your heart rate reserve) starts to shrink. This is why maintaining a low resting rate becomes even more vital as you hit your 50s and 60s—it gives you more "room" to move and exert yourself without hitting your ceiling.
How to Get an Accurate Reading
Don't trust a single data point. If you just walked up a flight of stairs and then sat down to check your watch, that’s not your resting rate. That’s your "sitting after walking" rate.
To get the real deal:
- Check it immediately upon waking.
- Don't look at your phone or check your email first (hello, stress spike).
- Lie still for at least two minutes.
- Take the average over five days.
Wearables are great for trends, but they can be finicky. Sometimes the green light sensor on a watch gets confused by tattoos, dark skin tones, or just a loose strap. If the number looks crazy, go old school. Two fingers on the radial artery (the thumb side of your wrist), count the beats for 30 seconds, and multiply by two. Simple. Effective.
Actionable Steps to Lower Your Baseline
If you've looked at your data and realized you're consistently higher than you'd like, you aren't stuck there. You can move the needle.
🔗 Read more: High Protein Vegan Breakfasts: Why Most People Fail and How to Actually Get It Right
Prioritize Magnesium and Potassium
These electrolytes are the "brakes" for your heart's electrical system. Most people are deficient in magnesium. Loading up on leafy greens, nuts, or a high-quality supplement (talk to your doctor first) can often settle a "jumpy" heart.
The Power of Zone 2 Cardio
You don't need to sprint until you puke. In fact, "Zone 2" training—exercise where you can still hold a conversation but you're definitely working—is the gold standard for strengthening the heart and lowering the resting pulse. Aim for 150 minutes a week of brisk walking, easy cycling, or swimming.
Breathwork is Real
It sounds "woo-woo," but five minutes of box breathing (inhale for 4, hold for 4, exhale for 4, hold for 4) directly stimulates the vagus nerve. This triggers the parasympathetic nervous system—the "rest and digest" mode—which sends an immediate signal to the heart to slow down. If you do this daily, you can actually retrain your baseline over time.
Watch the Caffeine Half-Life
Caffeine has a half-life of about 5-6 hours. If you have a cup at 4 PM, half of it is still buzzing in your system at 10 PM. This can keep your sleeping heart rate high, which prevents your body from truly recovering. Try a "caffeine cutoff" at noon for a week and watch what happens to your morning numbers.
Your average heart rate resting is a living, breathing stat. It’s a snapshot of your current lifestyle choices, your environment, and your genetics. Don't obsess over a single high reading, but do pay attention to the trend. If you’re consistently in the 50s or 60s and you feel energetic, you’re likely in a great spot. If you’re pushing 80 or 90 while sitting on the couch, it’s a clear signal to start making some of those small, boring, but incredibly effective lifestyle tweaks.
Start by tracking it for one full week. Use a pen and paper if you have to. Once you know your true baseline, you can finally stop guessing and start actually managing your cardiovascular health with a bit of precision.