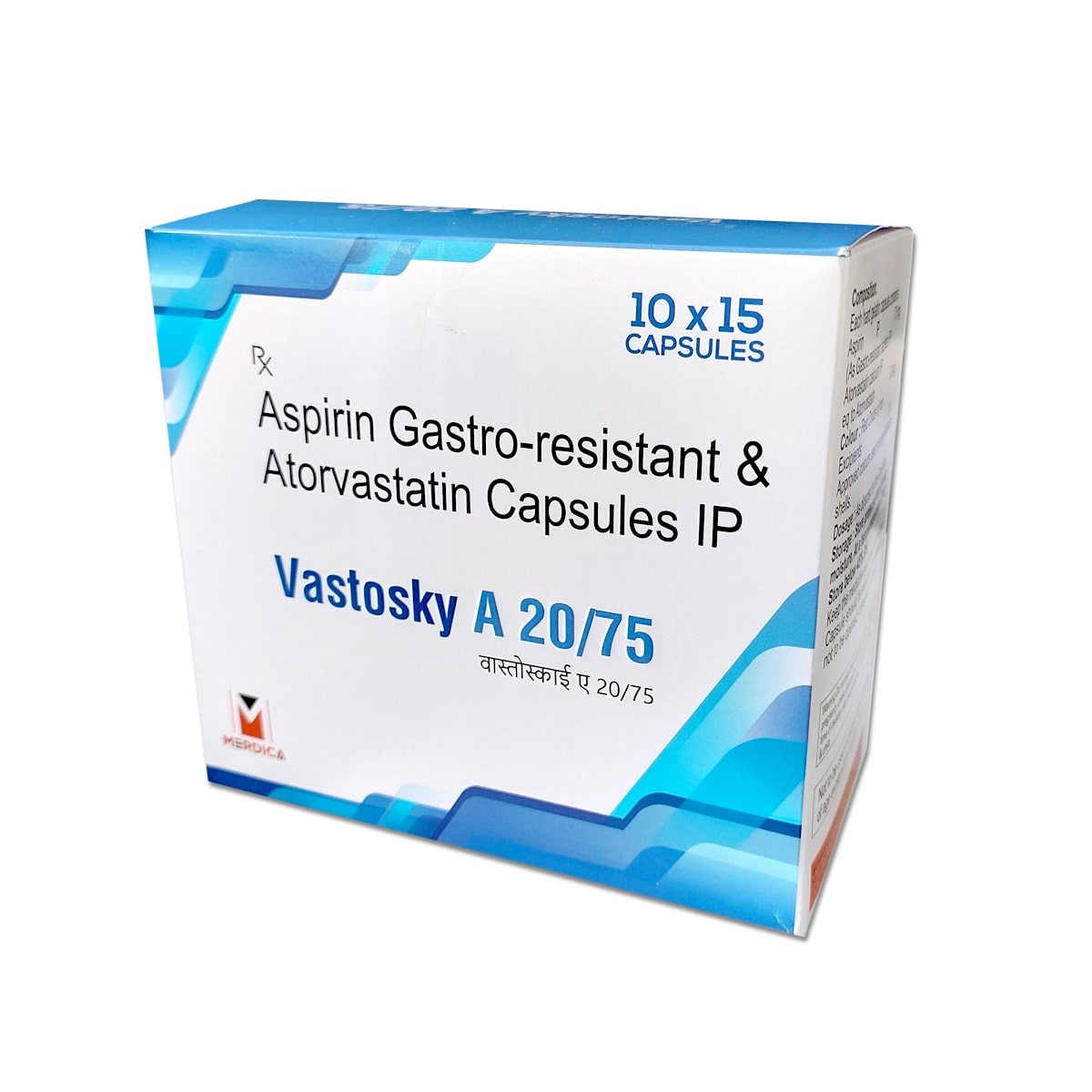
You’re staring at a small white tablet. Maybe you just picked up your first orange pill bottle from the CVS pharmacy counter, or perhaps you’ve been taking it for years and suddenly realized you don't actually know why. It’s a common scenario. Atorvastatin—brand name Lipitor—is one of the most prescribed drugs in the history of modern medicine. But when we talk about what is atorvastatin 20 mg used for, it’s not just about "lowering numbers" on a lab report.
It's about plumbing.
Think of your arteries like the pipes in an old house. Over time, gunk builds up. In your body, that gunk is cholesterol, specifically low-density lipoprotein (LDL). When a doctor hands you a prescription for a 20 mg dose, they aren't just trying to win a game of "get the LDL as low as possible." They are trying to stabilize the "pipes" so they don't burst or clog completely.
The 20 mg Sweet Spot: Why This Specific Dose?
Atorvastatin comes in a few flavors: 10 mg, 20 mg, 40 mg, and the heavy-hitting 80 mg. The 20 mg dose is often considered the "moderate-intensity" baseline. It’s the middle ground. Doctors often start here if your risk isn't sky-high, but your lifestyle changes—like those extra salads and morning walks—just aren't cutting it.
Basically, the 20 mg dose is designed to lower your LDL cholesterol by about 30% to 50%. That's a massive chunk. If your "bad" cholesterol is sitting at 150 mg/dL, this dose aims to drag it down into the double digits.
Why not just give everyone 80 mg and call it a day?
Side effects. Statins are generally safe, but they can be finicky. The higher the dose, the higher the risk of that annoying muscle ache known as myalgia. The 20 mg dose is often the "Goldilocks" zone—strong enough to provide significant cardiovascular protection, but gentle enough that most people don't feel like they’ve been hit by a truck the next morning.
✨ Don't miss: The Truth Behind RFK Autism Destroys Families Claims and the Science of Neurodiversity
It’s Not Just About Cholesterol
Here is the secret: Atorvastatin does things for your heart that have nothing to do with your cholesterol levels. This is a concept called "pleiotropic effects." It’s a fancy medical term that basically means the drug is a multi-tasker.
Even if your cholesterol was "normal," a doctor might put you on atorvastatin 20 mg because it’s an anti-inflammatory powerhouse. It stabilizes the plaque already living in your arteries. Imagine a blister. If that blister stays soft and "unstable," it can pop. In an artery, a popped "blister" of plaque causes a blood clot. That clot causes a heart attack. Atorvastatin acts like a metaphorical Band-Aid, calcifying that plaque and making it hard so it stays put.
- It improves "endothelial function." That's the ability of your blood vessels to relax and dilate.
- It reduces oxidative stress.
- It keeps your blood from getting too "sticky."
If you have Type 2 diabetes or existing heart disease, you aren't just taking this for the numbers. You're taking it for the "stability."
The Reality of Side Effects (And the Nocebo Effect)
Let's be honest. People are terrified of statins. You’ve probably read a horror story on a forum about someone who couldn't walk after three days on Lipitor.
Muscle pain is real, but it’s often overblown. Clinical trials, like the ASCOT-LLA study, have shown that while some patients definitely experience muscle issues, a huge portion of reported pain is actually the "nocebo" effect. That's the opposite of a placebo—you expect to feel bad, so your brain creates the sensation.
However, if you do get dark urine or "coke-colored" pee, stop. Call your doctor. That’s rhabdomyolysis. It’s incredibly rare (we’re talking 1 in 100,000 rare), but it’s the serious one where muscle tissue breaks down and stresses the kidneys.
🔗 Read more: Medicine Ball Set With Rack: What Your Home Gym Is Actually Missing
What's more common? A slight bump in blood sugar. For most, the heart-saving benefits far outweigh a tiny tick upward in glucose, but it’s why your doctor will keep an eye on your A1C levels during your checkups.
The Grapefruit Myth (And Other Rules)
You’ve heard it: "Don't eat grapefruit!"
Is it true? Yeah, kinda. Grapefruit contains furanocoumarins. These chemicals mess with the enzyme (CYP3A4) in your gut that breaks down atorvastatin. If the enzyme is "busy" dealing with the grapefruit juice, too much of the medication enters your bloodstream. It’s like turning a 20 mg dose into a 40 mg or 80 mg dose overnight. One half of a grapefruit probably won't kill you, but a giant glass of juice every morning is a bad idea.
Also, timing matters—but less with atorvastatin than older statins. Older drugs like simvastatin have a short "half-life," so you have to take them at night when your liver makes the most cholesterol. Atorvastatin lasts longer in the body. You can take it in the morning or at night. Just be consistent.
Who Is This Actually For?
The guidelines for who gets atorvastatin 20 mg changed significantly a few years ago. It used to be all about the LDL number. Now, it’s about your "10-year risk score."
Doctors use a calculator (the ASCVD Risk Estimator) that looks at your age, sex, blood pressure, smoking status, and whether you have diabetes. If your risk of having a heart attack in the next decade is over 7.5%, you’re likely getting a script.
💡 You might also like: Trump Says Don't Take Tylenol: Why This Medical Advice Is Stirring Controversy
- Primary Prevention: You haven't had a heart attack yet, but your risk factors are stacking up like a Jenga tower.
- Secondary Prevention: You’ve already had a "cardiac event." In this case, 20 mg might actually be a starting dose before they ramp you up to 80 mg.
- Familial Hypercholesterolemia: This is the genetic lottery nobody wants to win. Your body just makes too much cholesterol, no matter how much kale you eat.
Practical Steps for Living with Atorvastatin
If you've just started your 20 mg journey, don't just pop the pill and keep eating cheeseburgers. The drug works with your lifestyle, not instead of it.
Watch your CoQ10 levels. Some cardiologists suggest taking a CoQ10 supplement. Statins naturally deplete this enzyme in your muscles, which might contribute to that "heavy leg" feeling. It’s not a miracle cure, but many patients swear it helps with the transition.
Get your liver checked. About six weeks after starting, you’ll need a blood draw. Your doctor is looking at ALT and AST levels. A tiny jump is normal. A big jump means your liver isn't a fan of the drug, and you might need to swap to a different statin like rosuvastatin (Crestor).
Don't ignore the "aches." If your calves feel like you ran a marathon when you actually just sat on the couch, tell your doctor. You aren't "being a baby." Sometimes a simple switch to a different brand or a slightly lower dose solves everything.
The long game. Most people stay on this medication for life. It’s not an antibiotic where you finish the pack and you're "cured." High cholesterol is a chronic condition. Stopping the medication usually results in your numbers bouncing right back to where they started within a few weeks.
At the end of the day, atorvastatin 20 mg is a tool. It's an insurance policy for your circulatory system. It buys you time. It keeps your arteries flexible. It makes sure that the plaque you already have stays where it belongs—quietly tucked away in the arterial wall, rather than causing a crisis.
If you're worried, talk to your pharmacist. They often know more about the subtle side effects and drug interactions than the prescribing physician. Ask them about your other meds—specifically if you take any antifungals or certain antibiotics, as these can interact poorly with your 20 mg dose. Stay hydrated, keep moving, and keep an eye on those labs. Heart health is a marathon, and this little pill is just one of the tools helping you reach the finish line.
Keep a log of how you feel for the first month. Note any unusual fatigue or muscle soreness. This data is gold for your doctor. It allows them to fine-tune your treatment so you get the protection you need without sacrificing your quality of life.