It starts with a weird, tight sensation in the chest. Maybe you’re out for a jog or just sitting on a sofa near a very fluffy cat. Suddenly, the air doesn’t go in right. You try to take a deep breath, but your lungs feel like they’ve shrunk two sizes. That’s the reality for about 25 million Americans. If you’ve ever wondered about asthma: what is it, you’re basically looking at a chronic condition where your airways—those tiny tubes moving air in and out of your lungs—decide to overreact to, well, almost anything. They swell up, get clogged with mucus, and the muscles around them tighten like a vice. It’s scary. It’s frustrating. And honestly, it’s one of the most misunderstood respiratory conditions out there.
People often think asthma is just "having a hard time catching your breath" during gym class. It’s way more complex than that. It’s an inflammatory disease. Think of it like having sensitive skin, but on the inside of your lungs. When something irritates those airways, they go into a defensive crouch. This isn't a one-time thing; for most, it’s a lifelong gig.
💡 You might also like: Effects Too Much Protein: What Most People Get Wrong About High-Protein Diets
The Plumbing Problem: Asthma Explained Simply
Your lungs are like an upside-down tree. The trunk is your trachea, and it branches out into smaller and smaller tubes called bronchi and bronchioles. In a healthy person, these tubes stay wide open. But with asthma, three specific things happen that mess everything up.
First, there’s bronchospasm. This is when the tiny muscles wrapping around your airways constrict. Imagine someone pulling a drawstring tight on a hoodie. Second, there’s inflammation. The lining of the tubes gets red and swollen, which physically narrows the space air can move through. Third, your body starts overproducing mucus. This isn't the normal stuff that keeps your throat moist; it’s thick, sticky junk that plugs up the remaining narrow opening.
When you combine those three, you get the classic wheeze. That whistling sound? That’s literally the sound of air trying to force its way through a gap the size of a pinhole. It’s exhausting. Your body has to work ten times harder just to do something that should be automatic.
Why Does This Even Happen?
We don’t actually have a "smoking gun" for why some people get it and others don't. Science points toward a mix of genetics and environment. If your mom or dad has it, your odds go up. But there’s also the "Hygiene Hypothesis." Some researchers, like those published in the New England Journal of Medicine, suggest that our ultra-clean, modernized lives might be part of the problem. Because we aren't exposed to as many bacteria and parasites as kids, our immune systems get bored and start attacking harmless things like pollen or dust mites.
Common Triggers (That Aren't Just Pollen)
- Exercise-Induced Bronchoconstriction (EIB): You might only feel symptoms when you’re pushing your heart rate. This is super common in athletes.
- The "Thunderstorm Asthma" Phenomenon: This sounds like a myth, but it’s real. Big storms can shatter pollen grains into tiny particles that get sucked deep into the lungs, causing mass flare-ups in entire cities.
- Workplace Irritants: Bakers (flour dust), hairdressers (chemical fumes), and woodworkers often develop "occupational asthma" after years of exposure.
- Strong Emotions: Laughing too hard or crying can actually trigger a flare-up. It’s a cruel joke of biology.
Distinguishing Between the "Types"
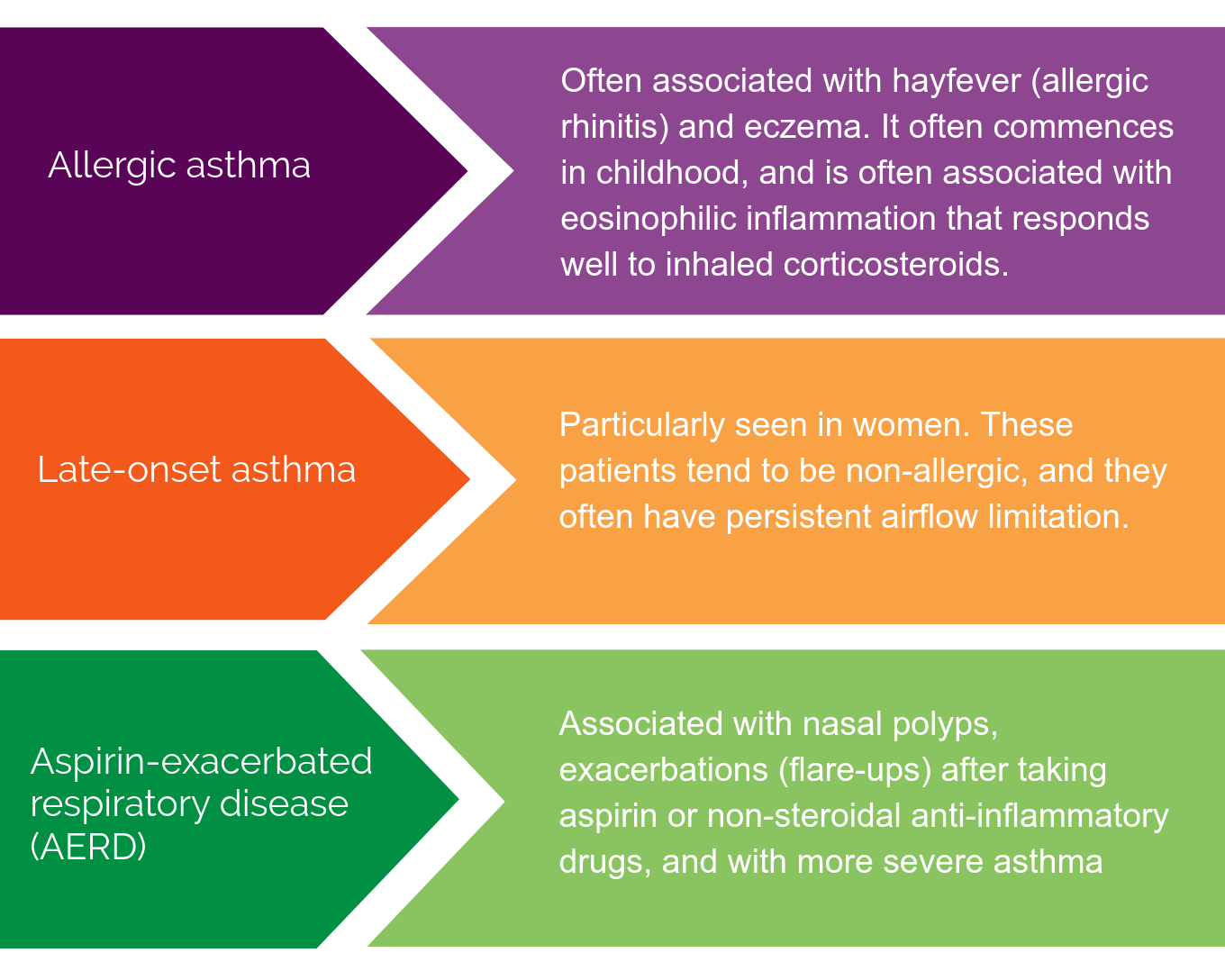
Not all asthma looks the same. You’ve got Allergic Asthma, which is the most common. This is the classic reaction to dander, mold, or dust. Then there’s Non-Allergic Asthma, triggered by things like cold air, viral infections, or even stress.
Some people deal with Eosinophilic Asthma. This is a more severe version driven by high levels of white blood cells called eosinophils. It often doesn't respond well to standard inhalers, which is why some patients feel like their medication "isn't working." It requires specialized biologics—targeted shots that block the specific proteins causing the inflammation.
The Scary Part: When Is It an Emergency?
Most people with asthma have a "rescue inhaler" (usually albuterol). It’s supposed to work in minutes. But sometimes, it doesn't. This is where we get into the territory of status asthmaticus. That’s a fancy medical term for an asthma attack that won’t quit.
If you see someone whose fingernails or lips are turning blue, or if they are "retracting" (the skin between their ribs or at the base of their neck is sucking in with every breath), that is a 911 situation. No questions asked.
Management Is More Than Just Puffing
There’s a huge difference between a Rescue Inhaler and a Controller Inhaler. Honestly, this is where most people mess up. A rescue inhaler is like a fire extinguisher. You use it when there's a fire. A controller (usually an inhaled corticosteroid) is like a sprinkler system. You use it every single day to prevent the fire from starting in the first place.
Many patients stop using their controllers because they "feel fine." But the inflammation is still there, simmering under the surface. Skipping that daily puff is like driving a car with thinning brake pads—you’ll be fine until you really, really need to stop.
Tools for Tracking
- Peak Flow Meters: This is a low-tech plastic tube you blow into. It measures how fast you can push air out. If your numbers start dropping, a flare-up is coming, even if you feel okay right now.
- Asthma Action Plans: Every patient should have a written plan from their doctor. Green zone means you’re good. Yellow means "increase meds." Red means "get to the ER."
- Smart Inhalers: Some new devices have Bluetooth sensors that track when and where you use your meds, helping doctors spot triggers you might have missed.
What Most People Get Wrong About Asthma
There is this lingering stigma that asthma is a sign of being "unfit" or "weak." That’s nonsense. David Beckham has asthma. Jackie Joyner-Kersee has it. It’s a physiological hurdle, not a character flaw.
Another misconception: "You'll grow out of it." While some kids do see their symptoms vanish during puberty, the underlying sensitivity often remains. It can roar back in your 30s or 40s after a bad bout of the flu or a move to a more polluted city.
Moving Toward Better Control
Living with asthma isn't about avoiding the world. It’s about prepping for it. You shouldn't have to quit soccer or stop hiking. If your asthma is limiting your life, it’s not "well-controlled." The goal of modern medicine isn't just to keep you alive; it's to make sure you forget you even have the condition most of the time.
Talk to your doctor about FeNO testing. It measures the amount of nitric oxide in your breath, which is a direct marker of how much inflammation is in your lungs. It’s much more accurate than just "listening" with a stethoscope.
💡 You might also like: Do Antibiotics Mess With Birth Control? The Truth Your Doctor Probably Didn't Explain
Actionable Steps for Managing Asthma Today
- Identify Your Personal Triggers: Keep a "symptom diary" for two weeks. Note the weather, what you ate, and if you were around animals. You might find a pattern you never suspected, like a specific cleaning spray or even scented candles.
- Check Your Inhaler Technique: Studies show up to 70% to 90% of people use their inhalers incorrectly. Most of the medicine hits the back of the throat instead of the lungs. Ask a pharmacist to watch you use it. Use a spacer if you use a metered-dose inhaler; it makes a massive difference in how much medicine actually reaches your airways.
- Vacuum with a HEPA Filter: Standard vacuums often just kick dust and allergens back into the air. A HEPA filter traps the tiny particles that actually trigger asthma.
- Get a Yearly Flu Shot: Respiratory viruses are the number one cause of asthma hospitalizations. Protecting your lungs from the flu or pneumonia is non-negotiable for asthmatics.
- Review Your Meds Every Six Months: Asthma is dynamic. Your needs in the winter might be totally different from your needs in the summer. Don't just stay on the same dose for a decade without checking in.