It starts as a tiny flicker of discomfort. You’re sitting at your desk or maybe lying in bed, and suddenly, there it is—that unmistakable, stinging pressure. Most of us know the drill. You drink a gallon of water, try some cranberry juice, and hope it goes away. It usually doesn't.
When you finally see a doctor, they’ll tell you it’s Escherichia coli. This bacterium is responsible for about 80% to 90% of uncomplicated urinary tract infections. It's basically the undisputed king of bladder misery. Because E. coli lives naturally in your gut, it’s always hovering nearby, waiting for a chance to migrate where it shouldn't be. Once it hits the urethra, the clock starts ticking. You need antibiotics for E coli UTI treatment because, frankly, your immune system often needs a heavy-hitter to clear out those sticky bacterial anchors.
Why E. Coli is Such a Persistent Jerk
E. coli isn't just floating around in your bladder like a piece of driftwood. It’s sophisticated. These bacteria have these tiny, hair-like projections called fimbriae. Think of them as microscopic grappling hooks. They latch onto the lining of your bladder so tightly that even a "flush" from drinking tons of water won't always dislodge them.
This is why the choice of medicine matters so much. If you pick the wrong one, or one the bacteria have seen before and learned to defeat, you’re just killing time while the infection climbs toward your kidneys.
The First-Line Defenders
In 2026, the medical community still leans heavily on a few tried-and-true options, but the "best" one has shifted lately due to resistance patterns. Nitrofurantoin—you might know it as Macrobid—is often the first thing a GP reaches for. It’s a bit of a specialist. Unlike other drugs that circulate through your whole body, Nitrofurantoin concentrates almost entirely in your urine.
It’s great because it hits the E. coli where they live without nuking your healthy gut bacteria as much as a broad-spectrum drug would. But there’s a catch. It doesn't penetrate tissue well. If the infection has moved into your kidneys (pyelonephritis), Nitrofurantoin is basically useless. You need something that gets into the bloodstream.
💡 You might also like: How Much Protein Does Hummus Have? The Honest Truth About Your Favorite Dip
Then there’s Fosfomycin. It’s a bit of a unicorn in the world of antibiotics for E coli UTI because it’s often a single-dose powder. You mix it with water, drink it, and it stays in your bladder for days. It's incredibly convenient, but honestly, some studies suggest it might not be quite as effective as a five-day course of Macrobid for certain stubborn strains.
The Problem With the "Big Guns"
We used to use Ciprofloxacin (Cipro) for everything. It was the easy button. But the FDA has issued several "Black Box" warnings about fluoroquinolones over the last few years. We’re talking about rare but serious side effects like tendon rupture or nerve damage. Doctors are much more cautious now. Unless your UTI is complicated or you’ve failed other treatments, you probably shouldn't be starting with Cipro.
Resistance is the other elephant in the room. E. coli is getting smarter. Or rather, we’ve been making it smarter by using the same drugs for decades. In many regions, the old standby Bactrim (Trimethoprim/Sulfamethoxazole) now faces resistance rates higher than 20%. If you live in one of those areas, taking Bactrim is basically like bringing a knife to a gunfight.
How Your Doctor Actually Picks Your Prescription
It isn't a guessing game, or at least it shouldn't be. A good clinician looks at your history. Have you had a UTI in the last six months? Did you travel recently? Have you been on antibiotics lately?
The gold standard is the urine culture.
They take your sample, grow the bacteria in a lab, and then literally drop different antibiotics on it to see which one kills the E. coli. This is called a sensitivity report. If you’re in a lot of pain, they’ll give you an "empiric" prescription—an educated guess—while waiting for the results.
- Nitrofurantoin (Macrobid): Usually 5 days. Minimal resistance. Good for simple cases.
- Trimethoprim-Sulfamethoxazole (Bactrim): 3 days. Fast-acting, but resistance is a major hurdle.
- Fosfomycin: One dose. Easy, but keep an eye on symptoms.
- Amoxicillin-Clavulanate (Augmentin): Used when others aren't an option, though E. coli is becoming quite resistant to penicillins.
The Dangers of "DIY" Antibiotic Use
I’ve seen people find an old bottle of Z-Pak (Azithromycin) in their cabinet and think, "Hey, this worked for my bronchitis, it’ll work for this."
Stop.
Azithromycin is not a standard treatment for E. coli UTIs. Taking the wrong drug doesn't just fail to cure you; it can actually mask the symptoms while the bacteria multiply. By the time you realize it didn't work, you might be dealing with a fever, back pain, and a trip to the ER for a kidney infection.
Also, don't stop taking your meds the second you feel better. We all do it. The burning stops on day two, and we forget the day three and four doses. This is exactly how you breed "superbugs." You kill off the weak bacteria first, leaving the strongest ones alive to replicate. Next time, that same antibiotic won't touch them.
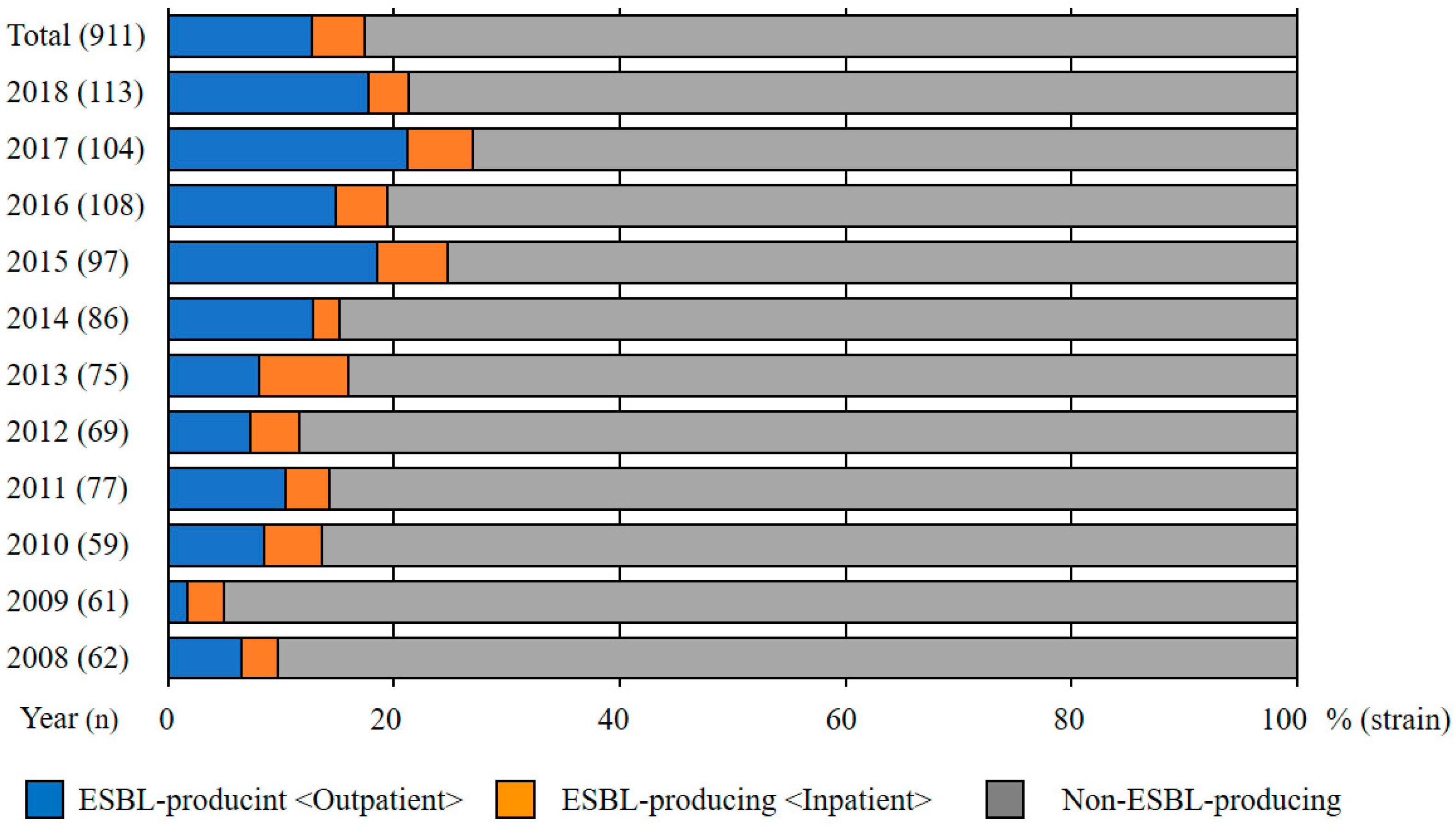
When Things Get Complicated: ESBL E. Coli
You might hear your doctor mention "ESBL." It stands for Extended-Spectrum Beta-Lactamase. It’s a fancy way of saying the E. coli has produced an enzyme that breaks down most common antibiotics like penicillins and cephalosporins.
If you have an ESBL infection, the standard antibiotics for E coli UTI list goes out the window. You might need IV drugs like Ertapenem or newer oral options like Pivmecillinam (which was recently approved by the FDA for use in the U.S.). This is why that urine culture I mentioned is so vital. You don't want to be fighting a futuristic superbug with 1970s tools.
Real Talk on Side Effects
Let’s be real: antibiotics can make you feel like trash. Nausea is the big one.
Macrobid is notorious for causing an upset stomach if you don't eat a big enough meal with it. And then there’s the yeast infection. Killing the bad bacteria in your bladder often kills the good bacteria in your vagina, leading to a whole new kind of itching and misery. Many women now ask for a "preemptive" dose of Diflucan (fluconazole) when they get their UTI meds just to avoid the secondary issue.
Probiotics are sort of a mixed bag. Some people swear by them to keep their gut balanced during treatment. The data is a bit "meh" on whether they actually prevent a yeast infection, but they certainly don't hurt. Just make sure you take the probiotic a few hours away from your antibiotic dose, or the medicine will just kill the expensive probiotics you just swallowed.
The Role of Cranberry and D-Mannose
Are they antibiotics? No. Can they help? Maybe.
D-Mannose is actually a type of sugar that looks a lot like the receptors on your bladder wall. The theory is that the E. coli grab onto the D-Mannose instead of your bladder, and then you just pee them out. It’s more of a preventative tool than a cure. If you already have a full-blown infection with a fever, D-Mannose is not going to save you. You need the pharmaceutical big guns at that point.
💡 You might also like: Why a 30 days arm workout challenge actually works if you stop obsessing over curls
What You Should Actually Do Now
If you're reading this while clutching a heating pad, here is your roadmap.
First, get to a clinic. Don't wait. A UTI can turn into a kidney infection faster than you’d think. Ask for a culture—don't just let them give you a random script if you've had multiple infections this year.
Once you have your antibiotics for E coli UTI, take them exactly as prescribed. Set an alarm on your phone. If you're taking Macrobid, eat a sandwich first. Drink an obscene amount of water to help the medicine reach every corner of the bladder.
Keep an eye out for "red flag" symptoms. If you start vomiting, get a high fever, or feel an intense ache in your lower back (near your ribs), your UTI might have moved up. That’s an emergency.
Finally, think about the "why." If this is your third UTI this year, talk to a urologist. It could be anything from your anatomy to your post-sex routine to the type of soap you're using.
Actionable Steps for Recovery:
- Confirm the Culprit: Ensure a urine culture is performed to verify it’s E. coli and not a resistant strain.
- Hydrate Aggressively: Aim for at least 2-3 liters of water a day to physically flush bacteria while the meds work.
- Complete the Cycle: Even if the pain vanishes in 24 hours, finish every single pill.
- Manage the Burn: Use Phenazopyridine (AZO) for the first 24 hours to numb the pain, but remember it masks symptoms—it doesn't cure the infection.
- Track Patterns: Record when your symptoms started and what you were doing (travel, new detergent, intercourse) to help your doctor identify triggers.
UTIs are a part of life for many, but they don't have to be a recurring nightmare if you treat the E. coli with the right respect—and the right prescription—the first time around.