You're sitting on the couch, maybe scrolling through your phone or watching a show, when you feel it. A weird tightness. A flutter. Suddenly, your brain kicks into overdrive and the only question that matters is: Am I having a heart attack? It is a terrifying thought. Honestly, it’s one of the most frequent reasons people end up in the emergency room only to find out they’re actually experiencing a panic attack or maybe just some really aggressive acid reflux. But you can't just ignore it.
Heart disease remains the leading cause of death globally, and according to the American Heart Association, someone in the US has a heart attack every 40 seconds. That’s a heavy statistic. It means that while the "false alarms" are common, the real thing is happening constantly. The problem is that Hollywood has lied to us. We expect the "Hollywood Heart Attack"—the dramatic clutching of the chest, the collapsing on the floor, the instant agony. In reality, it’s often much more subtle, especially for women, and that’s where the danger hides.
What a Heart Attack Actually Feels Like (It's Not Always Pain)
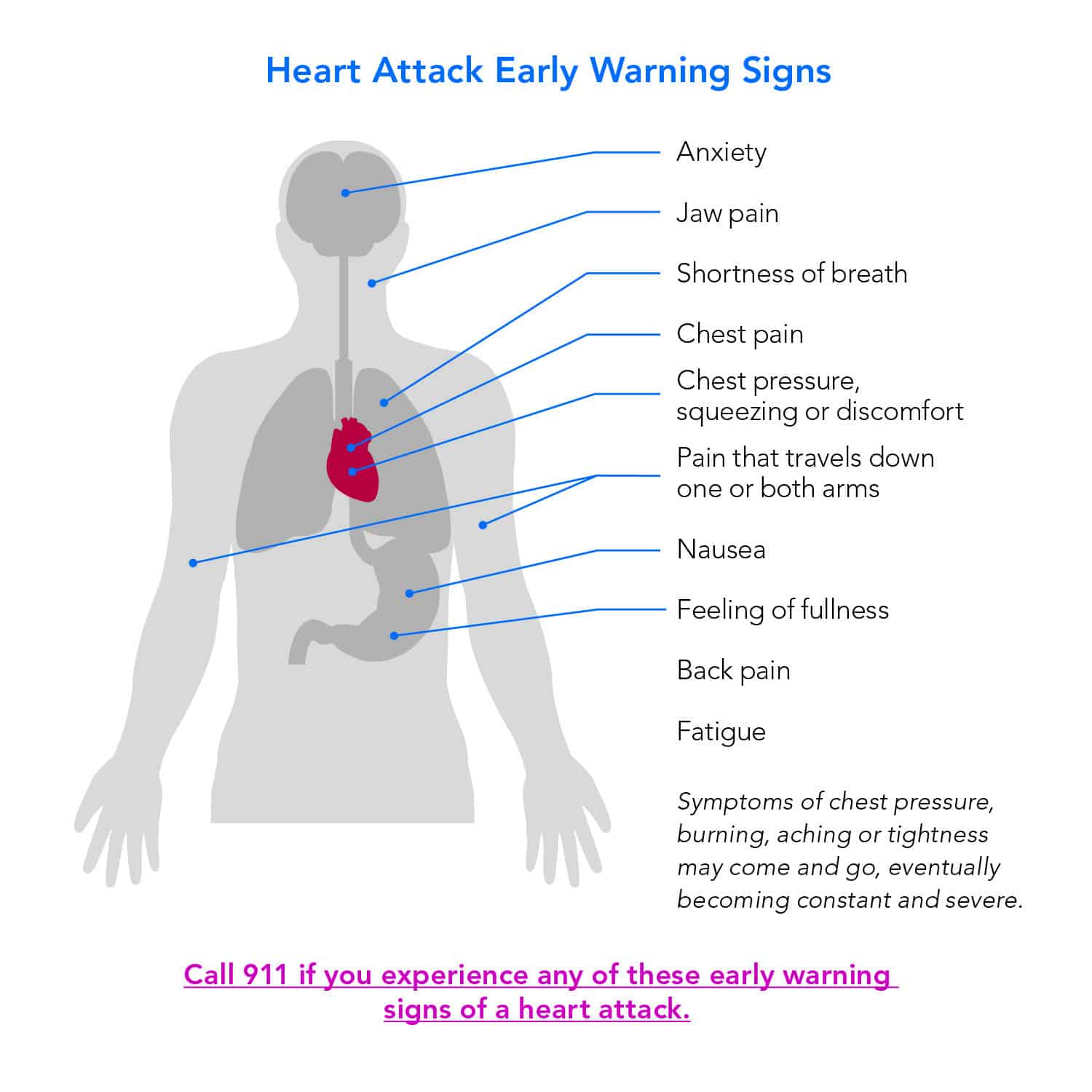
Most people expect sharp, stabbing pain. That happens sometimes, but more often, patients describe it as "pressure." It feels like an elephant is sitting on your chest, or like someone is tightening a belt around your torso. It’s a dull, heavy discomfort that doesn't go away when you change positions. If you can point to one tiny spot with your finger and say "it hurts right here," it’s actually less likely to be your heart and more likely to be a musculoskeletal issue. Heart pain is diffuse. It’s everywhere and nowhere at the same time.
💡 You might also like: Why Can You Bench Press a Person (and How Heavy Can They Really Get?)
It radiates. That’s the keyword. The discomfort often travels up into your jaw, down your left arm, or even into your back between the shoulder blades. I’ve talked to people who thought they just had a weird toothache or a pulled muscle in their neck, only to realize later their heart was struggling for oxygen.
The Silent Signs We Ignore
Then there’s the sweating. Not "I just ran a mile" sweating, but a cold, clammy drenching that comes out of nowhere. If you are sitting in a cool room and you’re suddenly soaked in a "cold sweat," that is a massive red flag. Combine that with a feeling of "impending doom." That sounds like a poetic exaggeration, but it’s a documented medical phenomenon. Your body knows something is wrong before your conscious mind catches up. You feel a profound sense of "I am going to die," and that instinct should never be ignored.
Nausea is another big one. A lot of folks, particularly older adults and those with diabetes, might just feel like they have a bad case of indigestion. They reach for the Tums when they should be reaching for the phone. This is why "Am I having a heart attack" is such a tricky question to answer alone; the symptoms mimic so many "normal" problems.
Why Women Experience This Differently
We need to talk about the gender gap in cardiology. For decades, medical research focused almost exclusively on men, leading to a "standard" set of symptoms that don't always apply to women. Women are less likely to report that crushing chest pressure. Instead, they might feel extreme, inexplicable fatigue. Imagine feeling so tired you can’t walk across the room, despite having slept eight hours.
Shortness of breath is also more prominent in women. It feels like you can't get a full lungful of air, even if you aren't exerting yourself. Dr. Nanette Wenger, a pioneer in geriatric cardiology at Emory University, has spent years pointing out that women’s symptoms are frequently dismissed as "anxiety" or "stress." If you feel like something is fundamentally wrong in your chest or breathing, and it doesn't fit the "crushing pain" mold, you still need to get checked.
Panic Attack vs. Heart Attack: The Great Mimic
Anxiety is a cruel beast. It can literally recreate the physical sensations of a cardiac event. When you have a panic attack, your sympathetic nervous system dumps adrenaline into your blood. Your heart rate spikes. Your chest tightens because your muscles are bracing for a "fight." You start hyperventilating, which causes tingling in your hands and around your mouth.
So, how do you tell?
Typically, a panic attack peaks within about 10 minutes and then begins to subside. A heart attack usually persists or comes in waves, getting progressively worse. Also, pay attention to the heart rate. A panic attack often sends the heart racing (tachycardia), whereas a heart attack might involve a racing heart, a slow heart, or even a completely regular rhythm. The biggest differentiator? If the pain gets worse with physical exertion—like walking up a flight of stairs—it is almost certainly cardiac. Panic attacks don't usually care if you're moving or sitting still; heart attacks do.
The Science of What's Happening Inside
Basically, a heart attack (myocardial infarction) happens when a coronary artery—one of the pipes supplying the heart muscle with blood—gets blocked. This is usually due to a buildup of plaque that suddenly ruptures, forming a clot.
When the blood flow stops, the heart muscle begins to die. Literally. Every minute that the vessel stays blocked, more muscle cells perish. This is why doctors say "time is muscle." If you get to a cath lab quickly, surgeons can use a balloon or a stent to open that pipe back up, saving the tissue. If you wait six hours because you "didn't want to be a bother," the damage might be permanent.
It’s worth noting that "cardiac arrest" and "heart attack" are not the same thing. Think of a heart attack as a plumbing problem (a blockage) and cardiac arrest as an electrical problem (the heart stops beating entirely). However, a plumbing problem can lead to an electrical problem.
What to Do Right Now if You're Worried
If you are reading this and honestly asking "Am I having a heart attack?" because you feel symptoms right now, stop reading and call 911. Or your local emergency number.
Don't drive yourself.
Don't have your spouse drive you.
Why? Because if your heart goes into an unstable rhythm while you're in the passenger seat of a Honda, your spouse can't do anything but pray. If you're in an ambulance, the paramedics have a defibrillator and cardiac meds ready to go. They can start treatment the second they walk through your front door.
The Aspirin Trick
If you're waiting for the ambulance, and you aren't allergic, chew one full-strength adult aspirin (325mg) or four baby aspirins. Chew it. Don't swallow it whole. Chewing gets the medicine into your bloodstream faster. Aspirin helps by thinning the blood and potentially slowing the growth of the clot that’s causing the blockage. It’s a simple move that has saved countless lives.
Risk Factors You Can't Ignore
We all know the basics: smoking, high blood pressure, and high cholesterol. But there are nuances. Chronic inflammation, measured by something called C-reactive protein (CRP), is a huge indicator that doctors are looking at more closely now. Sleep apnea is another silent killer; if you stop breathing at night, it puts immense strain on your heart.
Also, look at your family history. If your father had a heart attack at 45, your risk profile is completely different than someone whose parents lived to 90 with clean arteries. Genetics isn't destiny, but it is a blueprint you need to be aware of.
Common Misconceptions That Get People in Trouble
- "I'm too young." I've seen 25-year-olds have heart attacks due to rare genetic conditions or substance use. Age is a factor, but it’s not a shield.
- "The pain isn't that bad." Severity doesn't equal danger. Some of the most lethal "widow-maker" heart attacks start with a mild, nagging discomfort.
- "I'll wait until morning to see how I feel." Most heart attacks happen in the early morning hours when blood is "stickier." Waiting until the sun comes up is often the most dangerous decision you can make.
Actionable Steps for Heart Health
You don't have to live in fear, but you should live with awareness. If you're concerned about your risk, there are specific things you can do beyond just "eating better."
✨ Don't miss: Para qué sirve el citrato de magnesio: lo que tu cuerpo intenta decirte y nadie te explica
- Get a Calcium Score: This is a quick CT scan (often costing around $100) that measures the amount of calcified plaque in your coronary arteries. It’s way more predictive than just a cholesterol test.
- Know Your Numbers: Don't just know your "total cholesterol." Ask for your ApoB levels. Many cardiologists, like Dr. Peter Attia, argue that ApoB is a much more accurate marker for cardiovascular risk than the standard LDL-C.
- Invest in a Wearable: Tools like the Apple Watch or KardiaMobile can take a basic ECG. They aren't a replacement for a hospital-grade 12-lead ECG, but they can catch atrial fibrillation or other irregularities that might be precursors to trouble.
- The Stress Test: If you get winded easily, ask your doctor about a stress test. They’ll put you on a treadmill and watch your heart's electrical activity under pressure. It’s better to find a blockage during a controlled test than while you’re hiking in the woods.
Listen to your body. It is incredibly loud when it needs to be. If the question "Am I having a heart attack" keeps popping into your head, your intuition is trying to tell you something. Maybe it's just stress, and maybe it's just heartburn. But when it comes to the pump that keeps you alive, being "wrong" at the ER is a lot better than being "right" at home.
If you're currently feeling chest heaviness, unexplained sweating, or pain radiating to your jaw or arm, call emergency services immediately. Sit down, chew an aspirin, and unlock your front door so medics can get in easily. Do not wait for the symptoms to pass. Memory of a "false alarm" is a small price to pay for a lifetime of future heartbeats.