You've probably heard it a thousand times at dinner parties. "It’s actually good for my heart," someone says while pouring a second or third glass of Cabernet. For decades, the medical community sort of hummed along with this. There was this idea of the "French Paradox"—the observation that French people had lower rates of heart disease despite a diet rich in saturated fats, allegedly thanks to their wine consumption. But lately, the vibe has shifted. Hard.
If you’re wondering what can alcohol do to your heart, the answer isn't a simple "it’s bad." It’s more like a "it’s complicated, and the more we learn, the less 'safe' it looks."
We used to think there was a J-shaped curve. This theory suggested that complete abstainers had a slightly higher risk of heart issues than moderate drinkers, while heavy drinkers had the highest risk. Newer research, specifically large-scale genomic studies like those published in The Lancet or by the World Heart Federation, is poking massive holes in that. They’re finding that many of those "healthy moderate drinkers" were actually just wealthier, exercised more, and ate better. The alcohol wasn't the hero. It was just a passenger.
What alcohol can do to your heart rhythm
Ever woken up after a wedding or a long holiday weekend with your heart thumping like a trapped bird? Doctors call this "Holiday Heart Syndrome." It’s not just a cute name; it’s basically acute atrial fibrillation (Afib) triggered by ethanol.
Afib is when the upper chambers of your heart quiver instead of beating effectively. It’s messy. It’s also dangerous because when blood pools in those quivering chambers, it can clot. If that clot travels to your brain? That's a stroke.
The weird part is that you don't have to be a chronic alcoholic to experience this. Even a single "binge" session—defined as four or more drinks for women or five for men in a two-hour window—can irritate the heart’s electrical system. Alcohol is a toxin. It changes how electrolytes like potassium and magnesium move across your heart cell membranes. When those levels get wonky, the electrical "spark" that tells your heart when to beat starts misfiring.
👉 See also: Why Your Best Kefir Fruit Smoothie Recipe Probably Needs More Fat
The pressure is rising
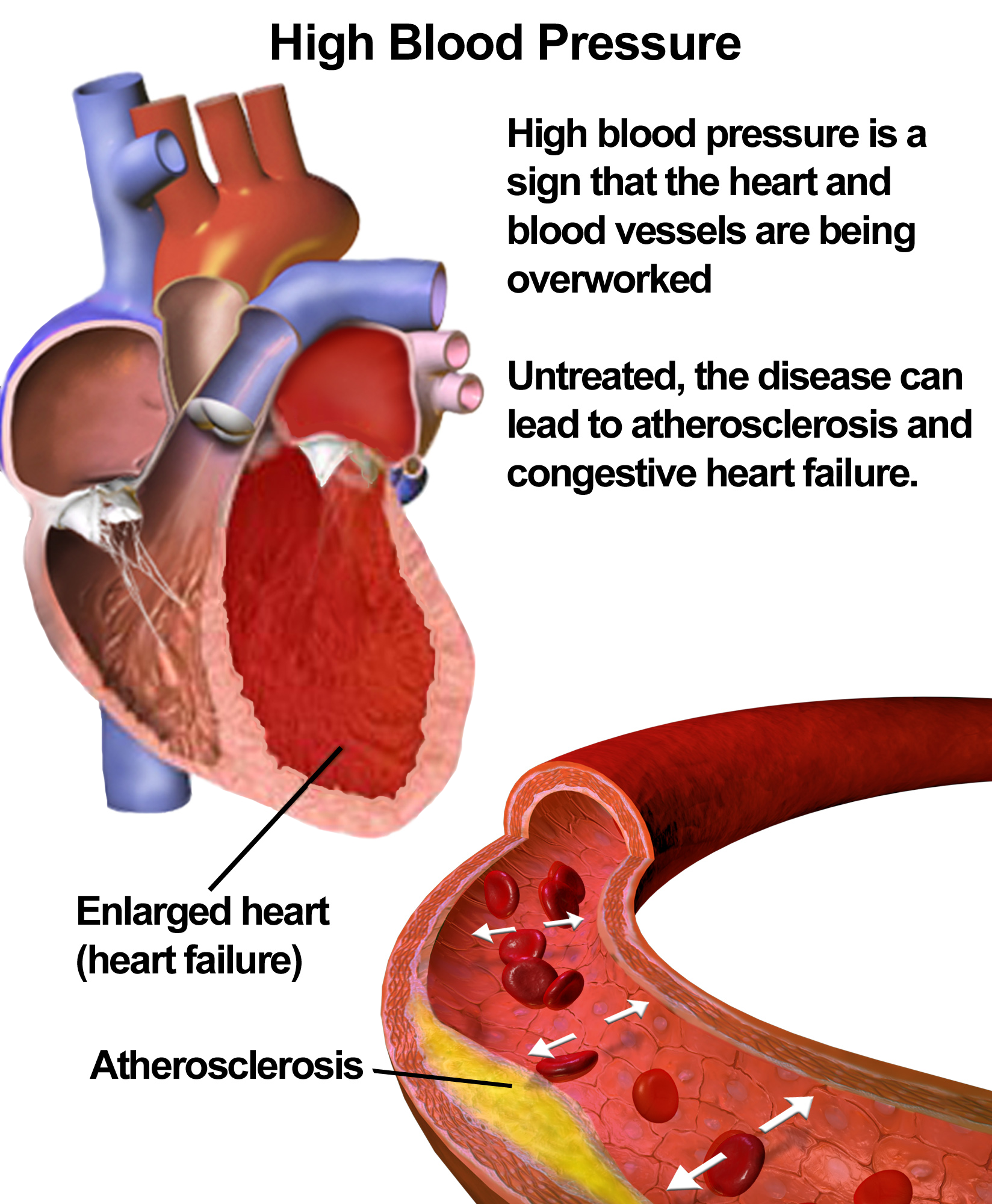
Blood pressure is arguably the most boring thing to talk about until it kills you. Hypertension is the "silent killer," and alcohol is one of its favorite accomplices.
When you drink, your body's sympathetic nervous system kicks into gear. This is your "fight or flight" mode. Your heart rate goes up, and your blood vessels constrict. While your BP might drop slightly immediately after a drink (vasodilation), the rebound effect is a spike.
If you're a regular drinker—even "just" two drinks a night—your baseline blood pressure often starts to creep up. Over years, this puts a massive strain on the arteries. They get stiff. They get scarred. This is a direct pathway to heart attacks. Dr. Timothy Naimi, a leading researcher formerly with the CDC, has pointed out repeatedly that the link between alcohol and increased blood pressure is one of the most consistent findings in all of nutrition science. There isn't really a "safe" amount for someone already struggling with hypertension.
Stretching the muscle: Alcoholic Cardiomyopathy
Imagine your heart is a rubber band. It’s designed to be snappy and strong. But if you keep stretching it out, eventually it loses its "boing." It becomes thin, floppy, and weak.
This is Alcoholic Cardiomyopathy.
✨ Don't miss: Exercises to Get Big Boobs: What Actually Works and the Anatomy Most People Ignore
This is usually reserved for the heavy hitters—people drinking excessively for years—but it’s a terrifying condition. When the heart muscle weakens, it can’t pump enough blood to the rest of the body. The heart tries to compensate by getting bigger (ventricular dilation), but that just makes it less efficient.
Symptoms start small. Maybe you're a little short of breath climbing the stairs. Maybe your ankles look a bit swollen at the end of the day. But eventually, it’s full-blown heart failure. The scary thing? Unlike some other forms of heart disease, this is 100% caused by the toxic effects of ethanol and its byproduct, acetaldehyde, on the heart cells (myocytes). The good news is that if caught early, the heart can sometimes repair itself—but only if the person stops drinking entirely. Not "cuts back." Stops.
The "Good Cholesterol" Myth
Let’s talk about HDL. For years, the pro-alcohol argument was that it raises your "good" cholesterol. While technically true, it’s a hollow victory.
Recent science has shown that not all HDL is created equal. The HDL you get from drinking doesn't actually seem to do the "scavenging" work that protects your arteries from plaque. It’s like hiring a security guard who looks the part but refuses to actually stop any intruders.
Furthermore, alcohol significantly raises triglycerides. These are fats in your blood. If you have high triglycerides and high LDL (the "bad" stuff), you’re basically building a wall of gunk inside your coronary arteries. It’s a recipe for a blockage.
🔗 Read more: Products With Red 40: What Most People Get Wrong
Is Red Wine still the exception?
Honestly, probably not. The resveratrol in red wine—the antioxidant everyone loves to cite—is present in tiny amounts. You would have to drink liters of wine every day to get the dose used in the laboratory studies that showed heart benefits. And by then, the liver damage and blood pressure spikes would far outweigh any antioxidant perks. You're better off eating a handful of red grapes or blueberries and skipping the fermentation.
Practical steps for a heart-healthy relationship with booze
If you're worried about what can alcohol do to your heart, you don't necessarily have to become a monk tomorrow. But the "moderate" goalposts have moved.
- Audit your "unit" size. A standard drink is much smaller than you think. It's 12 ounces of 5% beer, 5 ounces of 12% wine, or 1.5 ounces of 80-proof spirits. Most restaurant pours are 1.5 to 2 standard drinks.
- The 3-Day Rule. Try to have at least three consecutive alcohol-free days a week. This gives your heart and liver a chance to "reset" and prevents the chronic inflammation that leads to tissue damage.
- Don't drink for "Health." If you enjoy a glass of scotch, have it because you like it. But stop telling yourself it’s medicine. Accepting that it’s a calculated risk allows you to make better choices.
- Watch the mixers. Tonic water is loaded with sugar. Margarita mix is a calorie bomb. Sugar increases inflammation, which compounds the damage alcohol does to your vessels.
- Get a wearable. If you have an Apple Watch or a Whoop strap, look at your Heart Rate Variability (HRV) and resting heart rate after drinking. Seeing the data—how your heart struggles to recover overnight—is often the wake-up call people need.
The narrative that alcohol is a "heart tonic" is officially outdated. The American Heart Association and the World Health Organization have both tightened their stances. While the occasional drink is unlikely to be your undoing, the most heart-healthy amount of alcohol is, quite clearly, zero. If you choose to drink, do it with the lights on—knowing exactly how it impacts your pump.
Actionable Next Steps:
- Check your BP: Use a pharmacy kiosk or home cuff the morning after drinking to see your "rebound" pressure.
- Trial a "Dry Month": Notice if your resting heart rate drops. Most people see a 5-10 beat-per-minute improvement within two weeks.
- Prioritize Electrolytes: If you do drink, supplement with magnesium and potassium (through food like avocados and bananas) to mitigate the electrical interference in your heart rhythm.