You pop a pill, the burning stops, and you go back to your spicy wings or that late-night espresso. It feels like a miracle of modern chemistry. But for millions of people, those little purple or yellow capsules are a double-edged sword. Dealing with acid reflux meds side effects isn't just about reading the tiny print on the back of a CVS bottle; it’s about understanding how your body actually processes nutrients when you've basically turned off its primary digestive engine.
Stomach acid isn't the enemy. We’ve been conditioned to think it is because it hurts so bad when it splashes into the esophagus. But that acid is there to kill bacteria and break down minerals. When you kill the acid, you change the environment of your entire gut. It’s a trade-off. Sometimes it's a necessary one, especially if you're dealing with Barrett’s Esophagus or severe erosive esophagitis. Other times? You might be swapping a burnt throat for a whole host of other issues you didn't see coming.
The Nutrient Theft Nobody Talks About
If you’ve been on a Proton Pump Inhibitor (PPI) like Omeprazole or Nexium for more than a few months, your body is likely struggling to grab what it needs from your food. This is one of the most insidious acid reflux meds side effects. Your stomach needs a low pH—that's high acidity—to "unlock" certain vitamins and minerals.
Take Magnesium. The FDA actually issued a formal warning about this years ago. When your stomach is too alkaline because of the meds, your intestines can't absorb magnesium properly. You might start getting leg cramps. You might feel anxious or notice your heart skipping a beat. It’s not "just getting older." It’s literally a chemical deficiency caused by the drug.
Then there’s Vitamin B12. This one is a slow burn. Your body stores a lot of it, so you might not notice a drop for a year or two. But once those stores run dry? You’re looking at fatigue, tingling in your hands and feet, and even memory "fog" that looks a lot like early dementia. Dr. Susan Cheng and other researchers have noted that the lack of gastric acid prevents the release of B12 from the proteins in your food. Basically, you're eating the right stuff, but your body is just letting it pass right through.
Why Your Bones Might Be at Risk
It sounds wild that a stomach pill could break your hip. But the data is pretty clear. Long-term use of these medications is linked to an increased risk of bone fractures, particularly in the hip, wrist, and spine.
✨ Don't miss: Why Do Women Fake Orgasms? The Uncomfortable Truth Most People Ignore
Why? Calcium.
Calcium carbonate—the stuff in many supplements and fortified foods—requires a high-acid environment to dissolve and get absorbed. If you’re blocking acid 24/7, that calcium just stays a solid chunk and exits your system. Over a decade, that leads to thinning bones. The medical community calls it osteoporosis, but for a PPI user, it’s often just a direct consequence of the medication’s mechanism. Honestly, if you're on these long-term, you should be chatting with your doctor about bone density scans or switching to calcium citrate, which doesn't need as much acid to work.
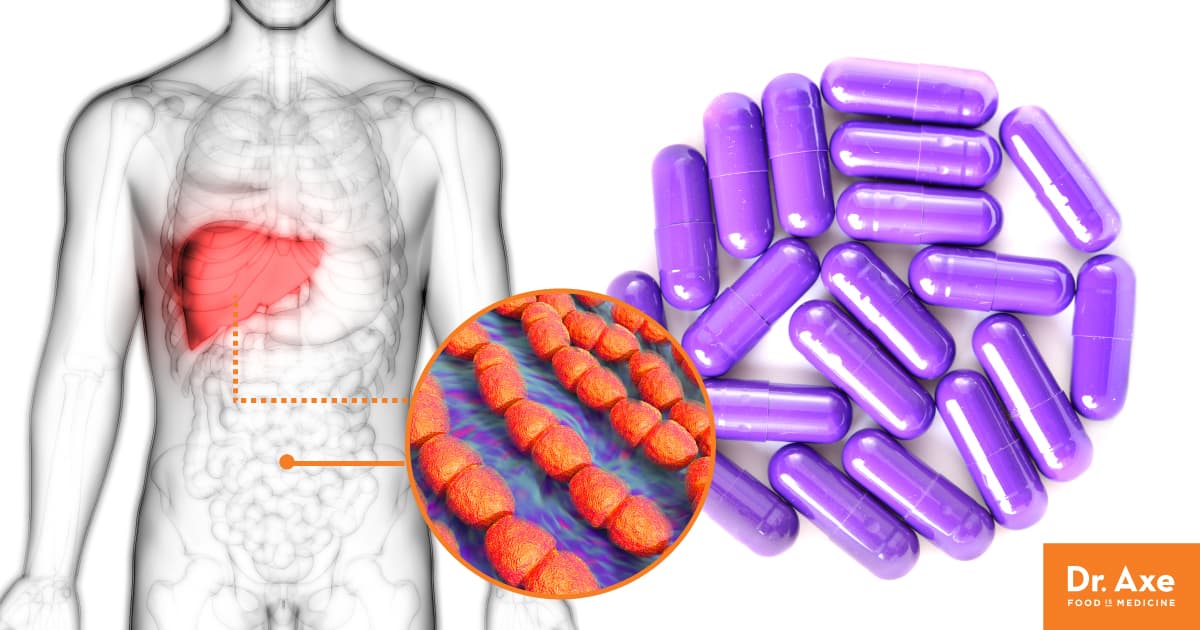
The Gut Microbiome Flip
Your stomach acid is your first line of defense against food poisoning and nasty bugs. It’s a vat of acid designed to kill invaders. When you neutralize it, you're essentially leaving the front door to your castle wide open.
One of the most serious acid reflux meds side effects is an increased risk of Clostridium difficile (C. diff) infection. This isn't just a "tummy ache." It’s a severe, sometimes life-threatening bout of diarrhea that is notoriously hard to treat. Without the acid barrier, C. diff spores can take root in your gut and go to town.
There’s also SIBO—Small Intestinal Bacterial Overgrowth. Normally, the stomach acid keeps the bacterial population in the small intestine in check. When the acid is gone, bacteria from the lower gut can migrate upward. You end up bloated, gassy, and miserable, wondering why your "reflux" meds are making your stomach feel like a balloon about to pop. It’s a weird irony: you take the pill to feel better, and you end up with a different kind of digestive nightmare.
🔗 Read more: That Weird Feeling in Knee No Pain: What Your Body Is Actually Trying to Tell You
Kidney Concerns and Sudden Shifts
For a long time, we thought PPIs were filtered out cleanly. Recent studies, including a large one published in JAMA Internal Medicine, suggest a link between long-term PPI use and chronic kidney disease (CKD).
It’s not entirely clear why. It could be repeated bouts of acute interstitial nephritis—basically a fancy way of saying the kidney gets inflamed as a reaction to the drug—that goes unnoticed until the damage is done. The scary part is that it often happens without any "symptoms" until the kidneys are functioning at a fraction of their capacity. If you're using these drugs like candy, you're putting a lot of "unpaid overtime" on your renal system.
The Rebound Effect: The Trap
This is the part that keeps people hooked. It’s called Rebound Acid Hypersecretion.
You decide you’ve had enough of the acid reflux meds side effects and you stop cold turkey. Suddenly, your heartburn is ten times worse than it ever was before you started the pills. You think, "Oh man, I really need this medicine! My reflux is terrible!"
Actually, your body is just overcompensating.
💡 You might also like: Does Birth Control Pill Expire? What You Need to Know Before Taking an Old Pack
When you block acid, your body produces a hormone called gastrin to try and force the stomach to make more. When you suddenly stop the drug, all those "acid-producing engines" that were being held back are suddenly floored. Your stomach floods with acid. It takes weeks, sometimes months, for the system to recalibrate. Most people give up after three days and go back on the meds, staying trapped in a cycle for years.
Managing the Risk Without Losing Your Mind
Does this mean you should go throw your meds in the trash? Probably not. If you have an active ulcer or a high risk of esophageal cancer, these drugs are life-savers. But for the average person with "a bit of heartburn" after a burger, there are smarter ways to play it.
- Tapering is king. Never, ever stop a PPI cold turkey. Work with a provider to slowly lower the dose while introducing H2 blockers (like Famotidine) which are generally considered "gentler" and have fewer long-term risks.
- Check your levels. If you're stuck on these meds, get your B12, Magnesium, and Ferritin (iron) levels checked annually. Don't wait for the symptoms.
- The 30-Minute Rule. Most people take PPIs wrong. They take them with food or at night. They need to be taken 30 to 60 minutes before your first meal of the day to actually work correctly. Taking them properly might allow you to use a lower dose.
- Mechanical fixes. Sometimes it’s not about the acid; it’s about the "door" (the LES) being weak. Elevating the head of your bed by six inches (with blocks, not just pillows) can do more for nighttime reflux than a pill ever will.
Actionable Next Steps
Start by tracking your triggers. It sounds cliché, but most reflux is driven by specific habits. If you're on a PPI, ask your doctor for a "step-down" plan. This usually involves moving from a PPI to an H2 blocker, then to an as-needed antacid.
Switch your calcium supplement to calcium citrate if you must stay on the meds, as it's better absorbed in low-acid environments. Lastly, consider a high-quality probiotic or fermented foods to help your gut microbiome stay resilient while your natural acid defenses are lowered. You have to be your own advocate here because, frankly, most 15-minute doctor appointments aren't long enough to cover the nuance of how these drugs change your long-term physiology.
Focus on the "why" of your reflux rather than just the "how" of stopping the burn. Whether it’s a hiatal hernia, a food sensitivity, or just a stressful lifestyle, addressing the root cause is the only way to truly escape the cycle of medication.