You’ve just left the doctor's office. In your hand is a lab report with a single number that feels like a final grade on your life. Maybe it’s a 7.2 or a 5.8. Honestly, it’s just a digit, but that digit determines if you're "well" or "uncontrolled" in the eyes of the medical establishment. This is the A1C, and while everyone talks about it, the standard a1c chart for diabetes often leaves out the most human parts of the equation.
It’s a three-month snapshot. Think of it like a long-exposure photograph of a busy street; you don't see the individual cars or the people tripping on the sidewalk, you just see the blurred average of the movement. That’s exactly what glycated hemoglobin is. It’s the sugar stuck to your red blood cells. Since those cells live for about 120 days, the lab can see how "sweet" your blood has been over the last season of your life.
But here’s the thing: people obsess over the chart. They stare at the grids and the percentages, trying to figure out if they’re failing. It’s not a test you pass or fail. It’s data. And frankly, the way we interpret that data is changing as technology like Continuous Glucose Monitors (CGMs) becomes more common.
Reading Between the Lines of an A1C Chart for Diabetes
The standard chart usually breaks things down into three buckets. If your number is below 5.7%, you're technically in the "normal" range. Between 5.7% and 6.4%, you’re in the prediabetes zone—a place that sounds scary but is actually a massive opportunity to pivot. Once you hit 6.5% or higher, that’s the diagnostic threshold for type 2 diabetes.
Wait.
There’s a massive catch.
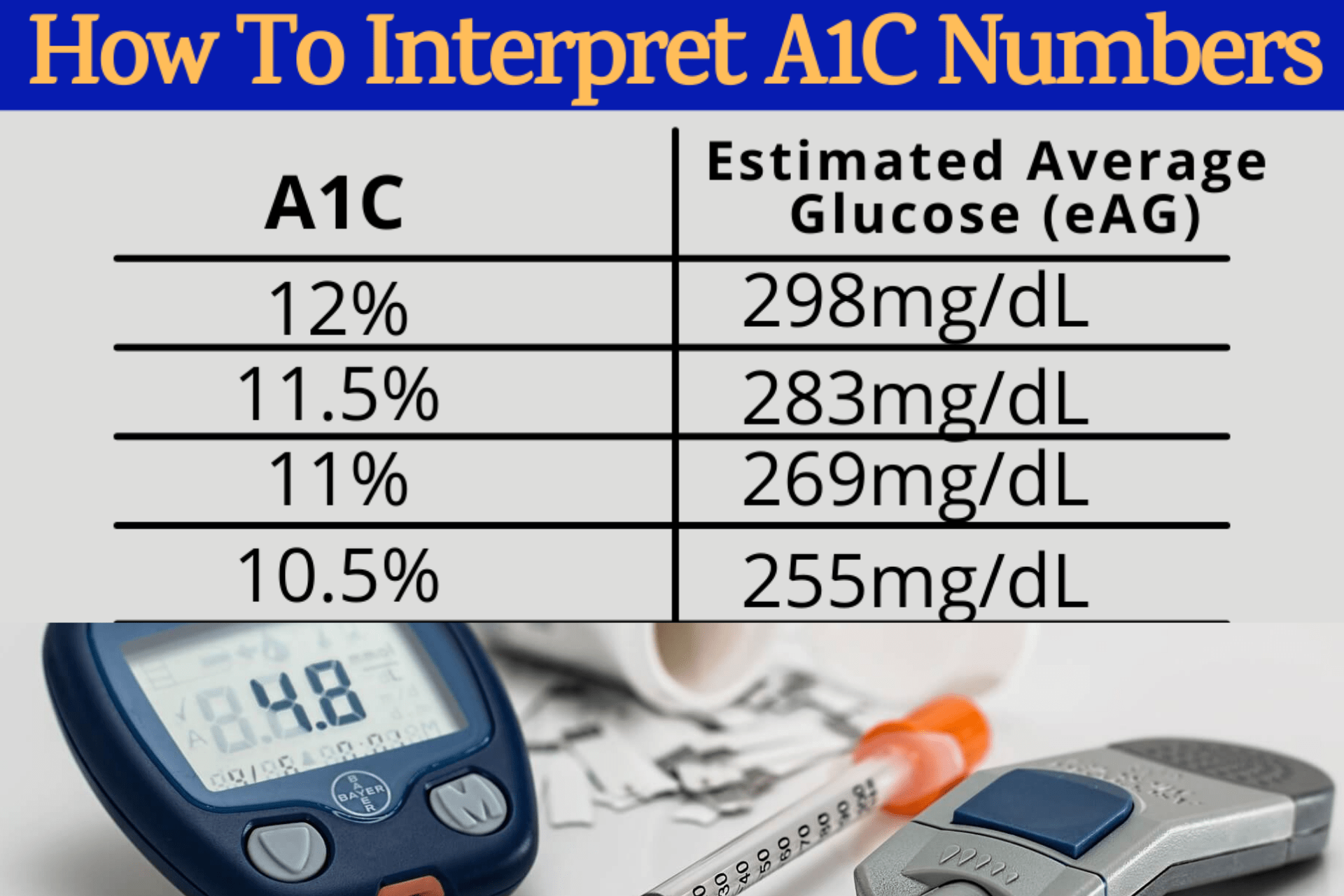
An A1C of 7% translates to an "estimated average glucose" (eAG) of about 154 mg/dL. Sounds simple, right? It isn't. You could be someone whose blood sugar stays perfectly flat at 150 all day and night. Or, you could be someone who swings violently from a dangerous 50 mg/dL to a skyrocketing 300 mg/dL. Both of you will have the exact same 7% on that a1c chart for diabetes.
✨ Don't miss: Why Do Women Fake Orgasms? The Uncomfortable Truth Most People Ignore
One of those people feels like garbage and is risking immediate complications, while the other is stable. This is why doctors like Dr. Irl Hirsch at the University of Washington have been vocal about the limitations of A1C. It doesn't show "Time in Range," which is arguably more important for how you actually feel on a Tuesday afternoon.
The Math Behind the Magic
If you want to do the mental gymnastics, the formula for eAG is $28.7 \times A1C - 46.7 = eAG$.
Don't worry about the math too much. Basically, for every 1% your A1C drops, your average blood sugar has decreased by about 29 mg/dL. That’s a huge win for your blood vessels.
Why Your Chart Might Be Lying to You
Not every body plays by the rules. If you have anemia, your red blood cells might not live as long as the "average" person's. If your cells die early, the sugar hasn't had time to stick to them. The result? A falsely low A1C. You think you’re doing great, but your actual blood sugar is high.
On the flip side, if you have certain vitamin deficiencies or kidney issues, your cells might live longer than 120 days. They collect more sugar over time, leading to a falsely high reading. It’s frustrating. You’re doing the work, eating the greens, walking the miles, and the paper still says you’re "out of control."
Pregnancy also messes with the numbers. Because of the rapid turnover of red blood cells and the changing volume of blood in a pregnant person's body, the A1C is often less reliable than the old-school finger pricks or glucose tolerance tests.
🔗 Read more: That Weird Feeling in Knee No Pain: What Your Body Is Actually Trying to Tell You
- Ethnicity matters too. Research has shown that African Americans, Latinos, and Asian Americans often have slightly higher A1C levels than Caucasians, even when their actual average glucose levels are identical.
- The "Glycation Gap." Some people are just "high glycators." Their bodies stick sugar to protein faster than others. It’s genetic.
- Age. As we get older, our "normal" A1C naturally creeps up. A 7.5% might be perfectly acceptable and safe for an 80-year-old, whereas a doctor would want a 30-year-old to be much lower to prevent long-term damage.
The Goalposts Move Based on Who You Are
The American Diabetes Association (ADA) generally recommends an A1C of below 7% for most non-pregnant adults. But that’s a guideline, not a law.
If you’re prone to severe hypoglycemia (low blood sugar), aiming for a 6.0% is dangerous. Going too low can lead to confusion, fainting, or worse. In these cases, a "looser" target of 8% is actually the smarter, safer medical choice. It’s about nuance. It’s about not chasing a number at the expense of your safety.
How to Actually Move the Needle
Forget "dieting." It's a miserable word. If you want to change what your a1c chart for diabetes looks like in three months, you have to look at the "Big Three": Muscle, Fiber, and Sleep.
Muscle is a glucose sponge. When you lift something heavy or do a few squats, your muscles can pull sugar out of your blood even without a ton of insulin. It’s like opening a side door to let the crowd out of a burning building.
Fiber is the brake pedal. If you eat a piece of white bread, that sugar hits your blood like a freight train. If you eat that same bread with a massive pile of broccoli and some avocado, the fiber and fat slow the absorption. The "spike" becomes a gentle hill.
And sleep? If you’re getting five hours a night, your cortisol is spiked. Cortisol tells your liver to dump sugar into your blood for energy you don't actually need because you're just sitting at a desk. You can eat perfectly and still have a high A1C because you’re stressed and exhausted.
💡 You might also like: Does Birth Control Pill Expire? What You Need to Know Before Taking an Old Pack
Real Talk on Medication
Sometimes, lifestyle isn't enough. And that's okay. Type 2 diabetes is a progressive, biological condition. Your pancreas might just be tired. Drugs like Metformin or the newer GLP-1 agonists (the Ozempics and Mounjaros of the world) are tools. Using a tool doesn't mean you failed; it means you're using the right equipment for the job. These medications work by changing how your body handles insulin or how quickly your stomach empties, directly impacting those peaks on the chart.
Actionable Steps for Your Next Checkup
Stop just looking at the number. When you see your doctor, ask for the context.
First, ask for your Estimated Average Glucose (eAG) alongside your A1C. It’s easier to visualize 140 mg/dL than 6.5%. It makes it feel more like a daily target and less like a grade.
Second, if your A1C doesn't match your finger-prick tests or how you feel, ask about a Fructosamine test. This looks at the last 2-3 weeks instead of 3 months. It’s a great way to see if recent changes are working or to bypass the red blood cell issues mentioned earlier.
Third, track your "Dawn Phenomenon." Many people find their A1C is high because their blood sugar spikes at 4:00 AM while they’re sleeping. No amount of "dieting" at dinner will fix a liver that's overproducing glucose in the middle of the night. You might need a specific adjustment to your evening routine or medication.
Finally, get a CGM if your insurance covers it (or if you can swing the out-of-pocket cost). Seeing the real-time reaction your body has to a bowl of pasta versus a bowl of berries is worth a thousand charts. It turns an abstract number into a lived experience. You start to see that a 15-minute walk after lunch can shave 40 points off your spike. That’s empowering.
The A1C chart is a map, but you are the one driving the car. Don't let a single coordinate on the map tell you that the whole trip is ruined. Take the data, adjust the steering wheel, and keep moving forward.