Most people think diabetes is just "the sugar disease." You either have the one you're born with or the one you get from eating too many donuts. That's a massive oversimplification that honestly hurts people. When we talk about the 5 types of diabetes, we’re really looking at five completely different ways the body's metabolic engine can stall out. It isn't just one thing. It's a spectrum of insulin issues, autoimmune attacks, and genetic quirks that require vastly different treatments.
If you treat Type 1 like Type 2, you end up in the ER. If you treat LADA like Type 2, you're just wasting time while your pancreas dies. Understanding these nuances is literally a matter of life and death for millions of Americans.
The classic autoimmune struggle: Type 1 Diabetes
Type 1 is the one everyone knows, or thinks they know. It's an autoimmune "friendly fire" situation. Your immune system decides the insulin-producing beta cells in your pancreas are invaders and wipes them out. It’s fast. It’s aggressive.
Commonly, it shows up in kids, which is why people used to call it "juvenile diabetes." That's a bit of a misnomer though. You can be 45 and suddenly your pancreas quits because of an adult-onset autoimmune response. There is no "lifestyle fix" for this. You can't kale-juice your way out of an autoimmune destruction of an organ.
You need insulin. Period. Without it, the body starts burning fat for fuel so fast it creates a toxic buildup of acids called ketones. This leads to Diabetic Ketoacidosis (DKA). It’s scary. It’s why Type 1 patients are some of the most data-literate people you'll ever meet—they have to be their own pancreas 24/7.
The metabolic giant: Type 2 Diabetes
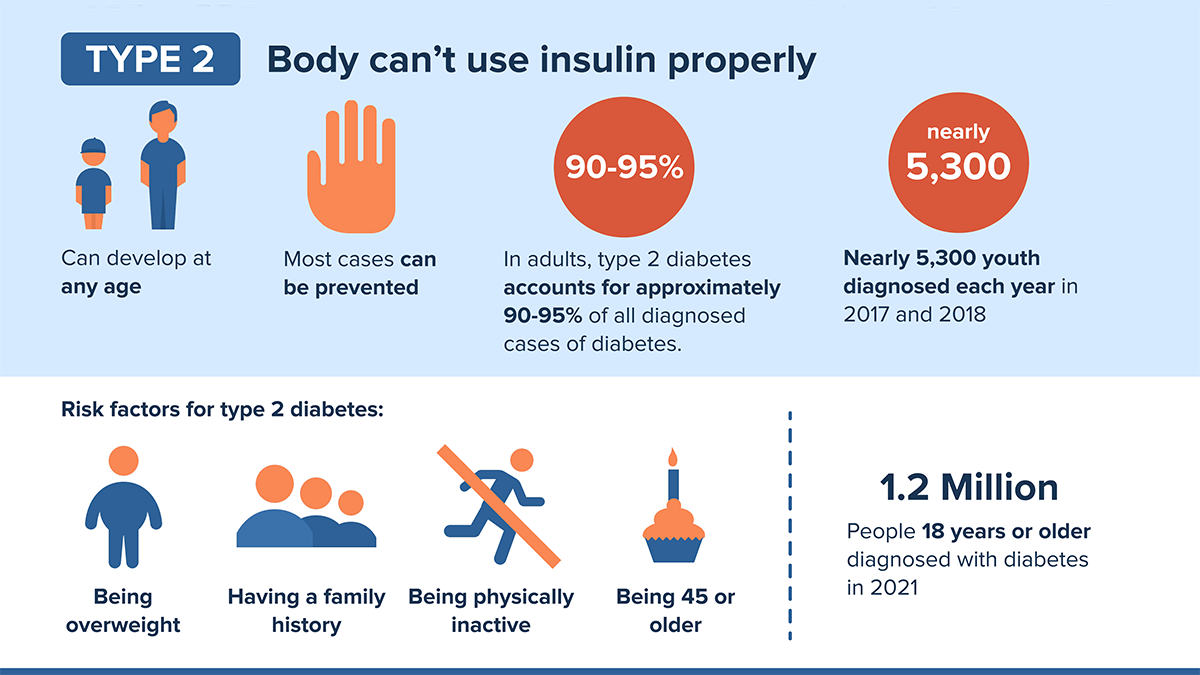
This is the big one. About 90% to 95% of all cases fall here. But here is what most people get wrong: it’s not always about weight. Genetics load the gun; environment pulls the trigger. In Type 2, your body still makes insulin (at least at first), but the cells just stop listening to it.
💡 You might also like: Is Tap Water Okay to Drink? The Messy Truth About Your Kitchen Faucet
It's called insulin resistance. Imagine a key trying to open a lock, but the lock is jammed with gum. The sugar stays in your blood, and your pancreas works overtime, pumping out more and more insulin to compensate. Eventually, the pancreas just gets tired. It burns out.
- The sneaky progression: Unlike Type 1, Type 2 can simmer for a decade before you notice.
- The "skinny" Type 2: There’s a subset of people with a "Thin on the Outside, Fat on the Inside" (TOFI) profile who have high visceral fat around their organs despite a low BMI.
- Reversibility? Doctors often debate the word "cure," but "remission" is definitely possible through radical carb reduction or bariatric surgery.
The "1.5" outlier: LADA (Latent Autoimmune Diabetes in Adults)
This is the most misdiagnosed version in the entire world of the 5 types of diabetes. LADA stands for Latent Autoimmune Diabetes in Adults. It’s basically Type 1 in slow motion.
Because it happens in adults, doctors almost always see a 40-year-old with high blood sugar and say, "Yep, Type 2. Here’s some Metformin." But Metformin doesn't stop an autoimmune attack. Patients with LADA might see their numbers improve for a few months, but then they hit a wall.
Why? Because their immune system is still killing those beta cells, just slowly. They don't need lifestyle changes as much as they need an early introduction to insulin to preserve whatever pancreatic function they have left. If you’ve been diagnosed with Type 2 but you’re fit, active, and your meds aren't working, you need to ask for a GAD antibody test. It’s the only way to know for sure.
The genetic fluke: MODY (Maturity-Onset Diabetes of the Young)
MODY is weird. It’s not autoimmune, and it’s not exactly insulin resistance. It’s a literal glitch in a single gene. If one of your parents has the MODY gene, you have a 50% chance of getting it.
📖 Related: The Stanford Prison Experiment Unlocking the Truth: What Most People Get Wrong
It’s often found in teens or young adults who aren't overweight and don't have the typical markers of Type 1. Because it’s a genetic mutation—specifically in genes like HNF1A or GCK—it behaves differently. Some forms of MODY don’t even need treatment; your "normal" blood sugar is just naturally higher than everyone else's, and it doesn't cause damage. Other forms respond incredibly well to cheap oral pills (sulfonylureas) rather than insulin injections.
Imagine taking shots for years only to find out a simple pill would have worked better because your doctor didn't realize you had a rare genetic variant. That's why family history is so crucial.
The temporary hurdle: Gestational Diabetes
Pregnancy is a massive stress test for the body. During the second and third trimesters, the placenta pumps out hormones that naturally cause insulin resistance. Usually, the mom’s pancreas just kicks into high gear to handle it.
But sometimes, it can’t.
That’s Gestational Diabetes. It usually goes away after the baby is born, but it’s a giant red flag for the future. Women who have had it have a significantly higher risk of developing "real" Type 2 later in life. It's like the body saying, "Hey, I can't handle this much metabolic stress."
👉 See also: In the Veins of the Drowning: The Dark Reality of Saltwater vs Freshwater
The risk isn't just for the mom; babies born to mothers with uncontrolled gestational diabetes are often larger (macrosomia) and have a higher risk of obesity and Type 2 themselves as they grow up. It’s a multi-generational metabolic issue.
What about Type 3c and Type 3?
Science is messy. While we officially focus on the primary categories, researchers like those at the Mayo Clinic and various Alzheimer’s institutes are now looking at "Type 3." This is a term used by some to describe Alzheimer’s as "diabetes of the brain," where brain cells lose their ability to use glucose.
Then there’s Type 3c, which is diabetes caused by physical damage to the pancreas—think pancreatitis, cystic fibrosis, or pancreatic cancer. If the organ is physically scarred or removed, it can't make insulin. It’s often mistaken for Type 2, but the treatment is much closer to Type 1.
Real-world action: Moving beyond the diagnosis
Knowing which of the 5 types of diabetes you are dealing with changes everything about your daily life. If you're struggling with management, you have to be your own advocate.
- Demand specific testing: If your diagnosis feels "off," ask for a C-peptide test (to see how much insulin you’re actually making) and an antibody panel (to check for autoimmune markers).
- Monitor more than just glucose: Keep an eye on your Time in Range (TIR). Modern Continuous Glucose Monitors (CGMs) are a game-changer for all types, not just Type 1.
- Check your family tree: If your family is full of "atypical" diabetics who aren't overweight, look into genetic testing for MODY.
- Muscle is medicine: For Type 2 and Gestational, resistance training is arguably more effective than cardio. Muscle tissue is the primary sink for glucose; the more you have, the more "buffer" your body has against blood sugar spikes.
- Mental health check: Diabetes distress is real. The mental load of tracking every carb and every movement is exhausting. Whether it’s Type 1 or Type 2, the "burnout" looks the same.
The bottom line is that the "sugar disease" label is an insult to the complexity of the human body. We are living in an era where we can pinpoint exactly why your metabolism is failing. Don't settle for a generic treatment plan that doesn't account for which specific version of this condition you're actually living with.