You're staring at a digital thermometer. It flashes 39°C. If you grew up with the metric system, you already know things are getting a bit dicey. But if your brain functions in Fahrenheit, you need an answer fast. Is this "take an aspirin and nap" territory, or "call the doctor immediately" territory?
Basically, converting 39 degrees celcius to farenheit puts you at exactly 102.2°F.
That’s not just a warm forehead. It’s a significant fever. When your body hits this specific number, it’s usually a sign that your immune system has moved past a minor skirmish and into a full-blown defensive war. It’s a high-grade fever.
Doing the Math (Without Losing Your Mind)
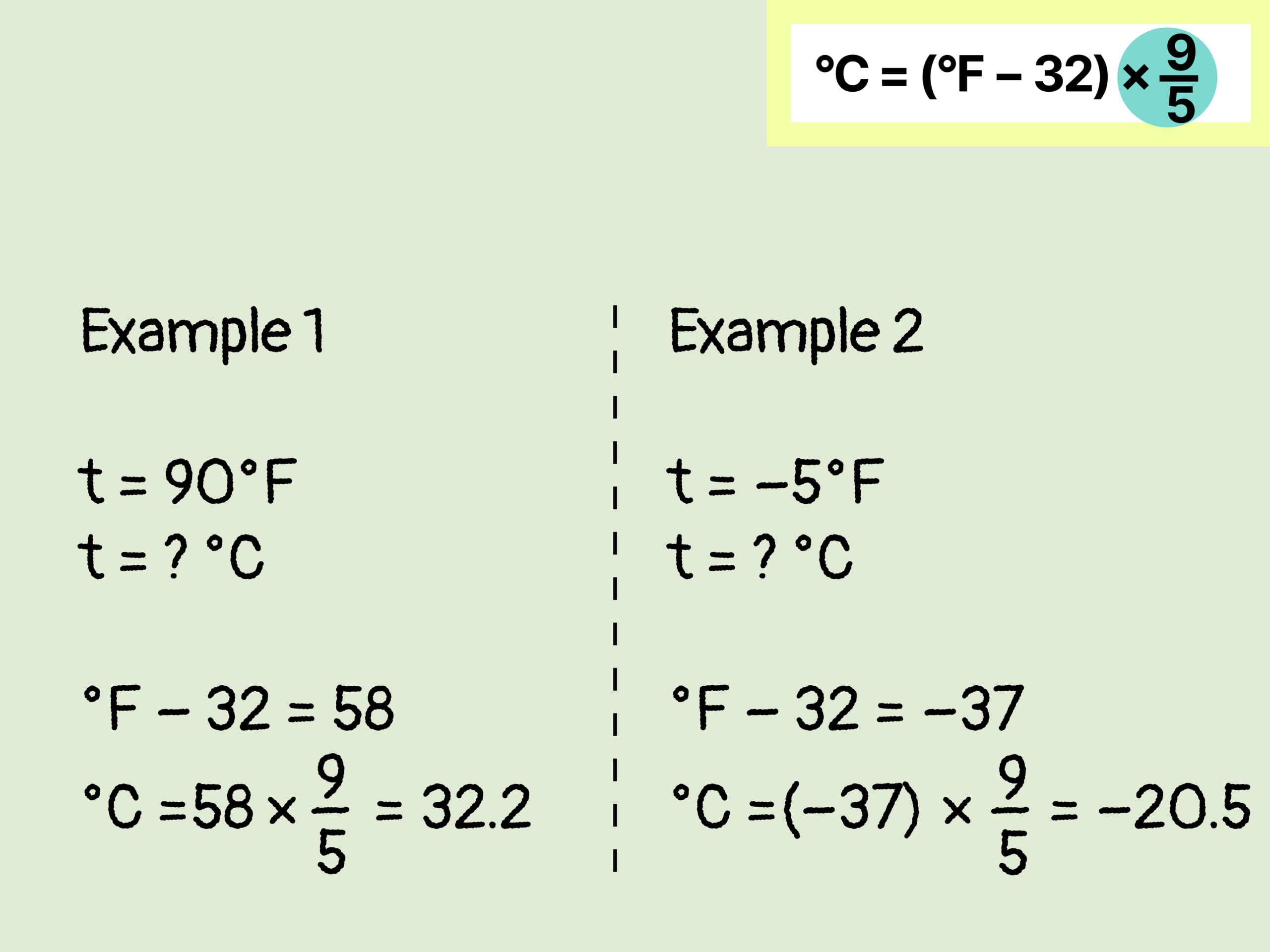
Most people just Google the conversion. I get it. But if you're stuck without signal or just curious how the gears turn, the math is actually pretty straightforward once you stop being intimidated by it.
The standard formula is $F = (C \times 1.8) + 32$.
Let’s walk through it. Take 39. Multiply it by 1.8. That gives you 70.2. Now, add 32. Boom. 102.2. Honestly, the easiest way to do it in your head when you're feeling sluggish is to double the Celsius number, subtract 10%, and add 32. Double 39 is 78. Ten percent of 78 is 7.8. Subtract that to get 70.2. Add 32. 102.2. It’s a bit of mental gymnastics, but it works every time.
The 39°C Threshold: What’s Happening Inside?
Medical professionals generally view a "normal" temperature as 37°C (98.6°F), though we now know that human averages have actually been dropping slightly over the last century. Some people naturally run cooler. But once you hit 39 degrees celcius to farenheit levels, the conversation changes.
At 102.2°F, your body is likely producing pyrogens. These are substances—sometimes produced by bacteria or viruses, sometimes by your own immune cells—that tell your hypothalamus to turn up the heat. Why? Because many pathogens struggle to replicate at higher temperatures. Your body is trying to cook the invaders.
However, there is a cost. At 39°C, your metabolic rate spikes. Your heart beats faster. You’re burning through fluids at an alarming rate. This is why you feel like you’ve been hit by a truck. You aren't just sick; you're physically exhausted from the internal heat production.
Is 39°C Dangerous?
It depends on who you are. Context is everything in medicine.
For a healthy adult, 102.2°F is miserable but usually not life-threatening if it stays there for a short duration. You’ll have the chills. You’ll probably sweat through your sheets. Your muscles will ache. But your brain isn't melting.
For an infant? Different story.
Pediatricians at places like the Mayo Clinic often advise that if a baby under three months has a temperature of 100.4°F (38°C) or higher, it’s an emergency. For older children, a 39°C fever is often managed at home unless it’s accompanied by lethargy, a rash, or a stiff neck. But that 102.2°F mark is often the "call the nurse line" threshold for parents.
The Misconception About "Breaking" a Fever
We’ve all heard it. "You need to sweat it out." People pile on five blankets when they hit 39°C.
Actually, don't do that.
👉 See also: St. John’s Episcopal: What You Need to Know About the Only Hospital in Far Rockaway Queens
Huddling under heavy blankets when you’re already at 102.2°F can actually drive your core temperature higher, which is the last thing you want. You want to help your body dissipate heat, not trap it. Light clothing and a cool room are your friends here. If you're shivering, a light sheet is fine, but don't turn yourself into a human burrito.
When 102.2°F Becomes a Problem
There’s a nuance here that gets lost in translation. A fever is a symptom, not the disease itself. If you take acetaminophen (Tylenol) or ibuprofen (Advil) and the number drops from 39 degrees celcius to farenheit's 102.2 down to 100 or 99, that’s a good sign. It means your body is still responsive to "antipyretics"—fever reducers.
If the fever stays pegged at 39°C or higher despite medication, or if it lasts more than a few days, that’s when doctors start looking for things like secondary bacterial infections, pneumonia, or UTIs.
Also, watch out for the "bounce." Sometimes you feel better in the morning, your temp drops to 37.5°C, and then by 6:00 PM, you’re back at 39.2°C. That’s the classic viral pattern. The evening spike is a jerk, but it’s common.
The Science of Measurement: Ear, Mouth, or Armpit?
Not all 39°C readings are created equal.
If you take a temperature under the arm (axillary), it’s usually about 0.5°C to 1°C lower than the actual core temp. So, if an armpit reading says 39°C, your internal temperature might actually be closer to 40°C (104°F). That’s a massive difference.
Oral readings are generally more accurate, provided you haven't just downed a hot coffee or an ice-cold Gatorade. Rectal readings remain the gold standard for accuracy in clinical settings, especially for kids, because they measure the core most directly.
Why Does 39°C Feel So Different From 38°C?
It’s only one degree, right?
In the Celsius world, one degree is a lot. Think about it: the entire range of "normal" to "deadly" is only about 5 or 6 degrees Celsius. Moving from 38°C (100.4°F) to 39°C (102.2°F) is a significant jump in energy expenditure.
At 38°C, you might feel "under the weather." At 39°C, you are likely bedridden. This is the point where "brain fog" sets in. You might find it hard to concentrate on a movie or even hold a complex conversation. Your body is diverting all resources to the immune front lines.
Actionable Steps for Dealing with 39°C (102.2°F)
If you or someone you're looking after hits this number, stop panicking and start managing.
First, hydrate like it’s your job. You are losing water through your breath and your skin at an accelerated rate. Water is fine, but something with electrolytes is better. Pedialyte isn't just for kids; it's a lifesaver for adults at 102.2°F too.
Second, track the timing. Don't just remember that it was high. Write down the time and the exact reading. When you're delirious with a fever, you will forget when you last took your meds. "Did I take the Advil at 2:00 or 4:00?" is a question you don't want to be guessing at.
Third, monitor for "Red Flag" symptoms.
A 39°C fever combined with a severe headache, a stiff neck, or sensitivity to light requires an immediate trip to the ER. These can be signs of meningitis. Similarly, if there’s a persistent cough or pain when breathing, you could be looking at pneumonia.
The Conversion Table You'll Actually Use
Since we're talking about 39 degrees celcius to farenheit, it helps to see the neighborhood.
- 38.0°C is 100.4°F (The entry-level fever)
- 38.5°C is 101.3°F (The "I'm definitely staying home" fever)
- 39.0°C is 102.2°F (The "This is getting serious" fever)
- 39.5°C is 103.1°F (The "Call the doctor" fever)
- 40.0°C is 104.0°F (The "Hospital" territory for many)
Environmental Heat vs. Internal Fever
It’s worth noting that if you’re looking up 39°C because of the weather and not a thermometer under your tongue, the advice changes. 39°C is a scorching day—about 102°F.
In this context, the danger isn't infection; it's heatstroke. If the air temperature is 39°C, your body can no longer cool itself effectively through sweat alone, especially if the humidity is high. When the "wet bulb" temperature gets too high, your internal temp will rise to match the environment.
Whether it's a fever or a heatwave, 39°C is a clear signal from nature (or your body) to slow down, find shade or a cool bed, and prioritize fluids immediately.
To manage a 39°C fever effectively, prioritize absolute rest and staggered fluid intake—aim for 250ml of electrolyte-rich liquid every hour while awake. If the temperature persists above 39°C for more than 48 hours without a downward trend, or if it fails to respond to over-the-counter fever reducers within 90 minutes of dosage, contact a healthcare provider to rule out underlying bacterial infections. Keep a log of temperature readings and any accompanying symptoms like rashes or respiratory distress to provide a clear clinical picture for a doctor.